Welcome to our Comprehensive BPH Treatment Guide, your go-to resource for enlarged prostate symptoms, medical and natural treatments, and lifestyle fixes.
“If you’re a man over 50, there’s a good chance you’ve experienced the frustrating symptoms of an enlarged prostate – frequent bathroom trips, weak urine flow, or that nagging feeling of incomplete emptying. The good news? You’re not alone, and there are effective ways to manage it.”
What is BPH?
Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland, a common part of aging for men. As the prostate grows, it can squeeze the urethra (the tube that carries urine), leading to bothersome urinary symptoms. While BPH isn’t life-threatening, ignoring it can worsen discomfort and even lead to complications like UTIs or bladder stones.
Why This Matters:
- 50% of men in their 50s and up to 90% by age 80 develop BPH.
- Symptoms can disrupt sleep, work, and quality of life – but they’re treatable.
- Early action helps prevent severe issues like kidney damage.
What’s Ahead:
This guide covers:
✔️ Causes and symptoms—know the warning signs.
✔️ Medical treatments—from medications to surgery.
✔️ Lifestyle fixes—diet, exercise, and habits for relief.
✔️ Natural remedies—what works (and what doesn’t).
“First, let’s break down why the prostate enlarges and how to recognize the symptoms.”
For answers to common questions, see our Comprehensive FAQ on Enlarged Prostate (BPH).
For a full index of articles on managing daily BPH discomfort and symptoms, visit our BPH Symptoms & Daily Management Silo Hub
2. Understanding BPH: Causes & Symptoms
“You don’t need to be a urologist to recognize the signs of an enlarged prostate—but understanding why it happens is the first step toward managing it effectively.”
What Causes an Enlarged Prostate?
BPH is primarily driven by hormonal changes and aging, but other factors play a role:
- Hormonal Shifts:
- Testosterone → DHT: As men age, testosterone converts to dihydrotestosterone (DHT), a hormone that stimulates prostate growth.
- Estrogen imbalance: Older men produce less testosterone but maintain estrogen levels, which may encourage prostate cell proliferation.
- Aging:
- By age 60, about 50% of men have BPH. By 85, that number jumps to 90% (Urology Care Foundation).
- Genetics & Family History:
- If your father or brother had BPH, your risk increases.
- Metabolic Factors:
- Obesity, diabetes, and heart disease are linked to worse BPH symptoms due to inflammation and poor circulation.
- Lifestyle Influences (Indirect):
- Sedentary habits may worsen pelvic congestion.
- Poor diet (high in red meat, low in veggies) could contribute to inflammation.
Common Symptoms of BPH
BPH symptoms vary from mild annoyances to severe disruptions. They’re often grouped as “obstructive” (blocked flow) or “irritative” (bladder irritation):
✅ Obstructive Symptoms:
- Weak urine stream (“dribbling”). If you are experiencing a weak stream, it is important to know 5 Causes Beyond BPH.
- Difficulty starting urination (hesitancy)
- Straining to pee
- Incomplete emptying (feeling like you’re not done)
✅ Irritative Symptoms:
- Frequent urination (especially at night—nocturia). Nighttime trips are a major quality-of-life issue; find practical advice in our guide to Nocturia Fixes.
- Sudden, urgent need to go
- Pain or burning (if a UTI develops)
🚩 Red Flags (See a Doctor ASAP):
- Blood in urine (could indicate infection or cancer)
- Inability to urinate (acute urinary retention—a medical emergency). Learn about the Long-Term Outlook for Untreated BPH and the serious risks of acute urinary retention.
- Kidney problems (back pain, fever, or swelling from backed-up urine)
Why Symptoms Worsen Over Time
- The prostate grows slowly, so symptoms may creep up unnoticed for years.
- Bladder muscles compensate at first, but eventually weaken, leading to worse retention.
- Untreated BPH can cause bladder stones, UTIs, or kidney damage.
“Now that you know the causes and warning signs, let’s explore the medical treatments that can help – from medications to minimally invasive procedures.”
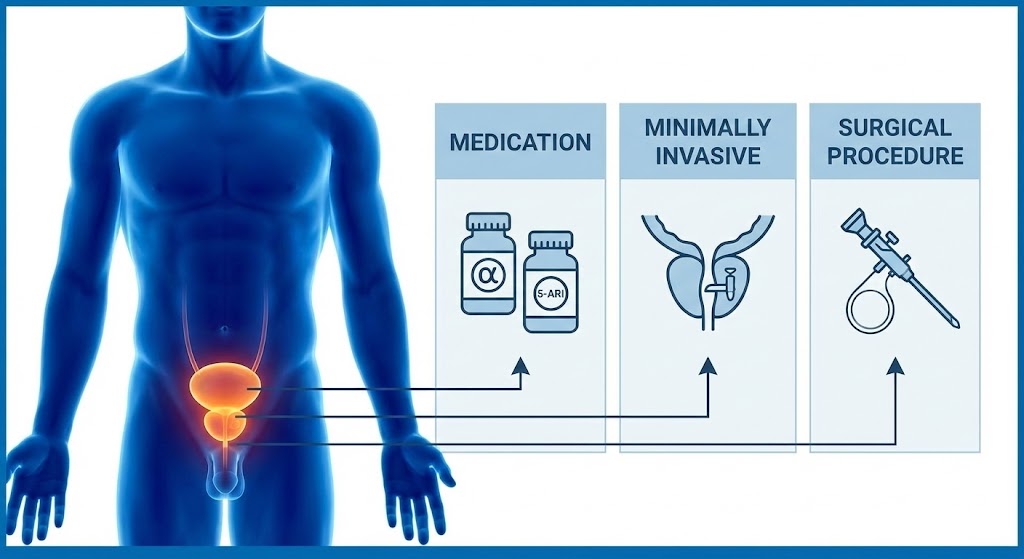
3. Medical Treatments for BPH: From Medications to Surgery
“When lifestyle changes aren’t enough to manage your enlarged prostate, modern medicine offers several effective solutions – from daily pills to minimally invasive procedures that can bring lasting relief.” Explore all surgical and pharmaceutical options in our BPH Medical & Surgical Treatments Silo Hub
A. Medications for BPH
1. Alpha-Blockers
- How they work: Relax prostate and bladder neck muscles to improve urine flow. The Mayo Clinic notes these drugs typically relieve symptoms within 1-2 weeks.
- Common options:
- Tamsulosin (Flomax)
- Alfuzosin (Uroxatral)
- Silodosin (Rapaflo)
- Pros: Work quickly (within days), good for moderate symptoms.
- Cons: May cause dizziness, low blood pressure, or retrograde ejaculation (dry orgasm).
2. 5-Alpha Reductase Inhibitors (5-ARIs)
- How they work: Block DHT (the hormone that grows the prostate), shrinking it over time.
- Common options:
- Finasteride (Proscar)
- Dutasteride (Avodart)
- Pros: Reduce prostate size by 20-30% after 6+ months; lower long-term risk of BPH complications.
- Cons: Slow to work (3–6 months); may cause sexual side effects (low libido, ED).
3. Combination Therapy
- For severe BPH: Alpha-blocker + 5-ARI (e.g., Flomax + Avodart).
- Best for: Men with large prostates and worsening symptoms.
4. Other Medications
- Anticholinergics (e.g., oxybutynin): For overactive bladder symptoms.
- Tadalafil (Cialis): Originally for ED, but also helps BPH by relaxing smooth muscles. We explore this dual-purpose medication in depth in Tadalafil (Cialis) for BPH
B. Minimally Invasive Procedures
1. TURP (Transurethral Resection of the Prostate)
- Gold standard surgery: A scope removes obstructing prostate tissue.
- Pros: Highly effective; symptoms improve in >90% of men.
- Cons: Requires anesthesia; risks include bleeding, retrograde ejaculation.
2. Laser Therapies
- GreenLight PVP (Photoselective Vaporization): Laser vaporizes prostate tissue.
- HoLEP (Holmium Laser Enucleation): Removes large prostates with minimal bleeding.
- Pros: Less bleeding than TURP; shorter recovery.
3. UroLift
- How it works: Tiny implants lift and hold the prostate away from the urethra. Read our full breakdown of the procedure, recovery, and comparison to TURP in UroLift for BPH: Pros, Cons, and What to Expect
- Pros: No cutting, preserves ejaculation, quick recovery (1–2 days).
- Cons: Not for very large prostates; may need repeat procedures.
4. Rezūm Water Vapor Therapy
- How it works: Steam destroys excess prostate tissue. For a detailed look at this innovative, office-based treatment, see our guide on Rezūm Water Vapor Therapy
- Pros: Office-based procedure; preserves sexual function.
C. Surgery (For Severe Cases)
1. Open Prostatectomy
- For very large prostates (>80g): Surgeon removes tissue through an abdominal incision.
- Pros: Most effective for extreme BPH.
- Cons: Longer recovery; higher risk of complications.
2. TUMT/TUNA (Older Therapies)
- Microwave/radiofrequency heat to shrink the prostate.
- Rarely used now (less effective than lasers/UroLift).
Which Treatment is Right for You?
| Option | Best For | Recovery Time | Sexual Side Effects? |
|---|---|---|---|
| Medications | Mild-moderate symptoms | N/A | Possible (especially 5-ARIs) |
| UroLift | Small-mid prostates, preserving ejaculation | 1–2 days | Rare |
| Laser (HoLEP) | Large prostates, long-term relief | 1–2 weeks | Low risk |
| TURP | Severe symptoms, gold standard | 2–4 weeks | Retrograde ejaculation common |
“While medical treatments are powerful, lifestyle changes can significantly boost your results – and may even slow prostate growth. Let’s dive into the best diet, exercise, and daily habits for BPH relief.”

4. Lifestyle Changes to Manage BPH: Diet, Exercise & Daily Habits
“Medications and procedures aren’t the only ways to fight BPH—simple lifestyle tweaks can significantly ease symptoms, boost treatment effectiveness, and even slow prostate growth. Here’s what really works.” Dive deeper into natural relief options, supplements, and exercise routines in the Natural Remedies & Lifestyle Silo Hub
A. Diet: Foods to Eat and Avoid
1. Best Foods for Prostate Health
- Lycopene-rich foods: Tomatoes (cooked), watermelon, pink grapefruit (lycopene reduces inflammation). We examine the link between diet and long-term health in Lycopene & Prostate Cancer Prevention.
- Zinc sources: Pumpkin seeds, oysters, lentils (zinc supports prostate function).
- Omega-3s: Fatty fish (salmon, sardines), flaxseeds (fight inflammation).
- Cruciferous veggies: Broccoli, cauliflower, Brussels sprouts (contain sulforaphane, linked to lower BPH risk).
- Berries & green tea: High in antioxidants that protect prostate cells.
2. Foods to Limit or Avoid
- Caffeine (coffee, tea, soda): Irritates the bladder, worsening urgency. Get the full moderation guide in Is Caffeine & Alcohol Really Bad for BPH?
- Alcohol: Increases urine production and nighttime trips.
- Spicy/acidic foods: Tomatoes (raw), citrus, chili peppers can aggravate symptoms.
- Processed meats & dairy: High-fat diets may worsen BPH progression.
3. Hydration Tips
- Drink plenty of water (but space it out—avoid gulping large amounts at once).
- Stop fluids 2–3 hours before bed to reduce nocturia.
B. Exercise & Movement
1. Aerobic Exercise
- Why it helps: Improves circulation, reduces inflammation, and may lower DHT levels.
- Best options: Brisk walking (30 min/day), swimming, cycling.
- Bonus: Helps maintain a healthy weight (obesity worsens BPH). Find out Best Forms of Exercise for BPH (and 3 Exercises to AVOID).
2. Pelvic Floor (Kegel) Exercises
- How to do them: Clench the muscles that stop urination midstream, hold for 5 sec, release. Repeat 10–15x, 3x/day. For step-by-step instructions, see Pelvic Floor Exercises for BPH.
- Benefits: Strengthens bladder control, reduces urgency.
3. Avoid Prolonged Sitting
- Take breaks every hour to walk/stretch – sitting compresses the prostate.
- Try a standing desk if you work sedentarily.
C. Bladder Training Techniques
1. Scheduled Voiding
- Method: Gradually increase time between bathroom trips (e.g., from every 1 hour to every 2).
- Goal: Train your bladder to hold more urine.
2. Double Voiding
- How: After urinating, wait 30 seconds, then try again to fully empty the bladder.
3. Stress Management
- Why: Anxiety exacerbates urinary urgency.
- Try: Deep breathing, yoga, or meditation to calm the nervous system.
Read about The Role of Stress Management in Reducing BPH Flare-Ups.
D. Other Practical Tips
- Limit decongestants & antihistamines: These can tighten urethral muscles, worsening obstruction.
- Wear easy-to-remove clothing: Avoid zippers/buttons if urgency is an issue.
- Elevate your legs while sitting: Reduces pelvic pressure.
Lifestyle vs. Medications: What to Expect
| Change | Potential Benefit | Time to See Results |
|---|---|---|
| Diet tweaks | Reduced inflammation, fewer symptoms | 2–4 weeks |
| Kegels | Better bladder control | 4–6 weeks |
| Aerobic exercise | Improved urine flow, weight loss | 6–8 weeks |
| Fluid management | Fewer nighttime bathroom runs | 1–2 weeks |
“For those seeking natural alternatives, certain herbs and supplements show promise—but not all are backed by science. Let’s separate fact from fiction in the world of BPH home remedies.”
5. Natural & Alternative Remedies for BPH: What Works and What Doesn’t
“Before you reach for that bottle of saw palmetto or try the latest ‘prostate miracle cure,’ know this: some natural remedies help BPH symptoms, while others are a waste of money – or even risky. Here’s the science-backed truth.”
A. Herbal Supplements with Scientific Support
1. Saw Palmetto (Serenoa repens)
- The Evidence:
- May block DHT (like finasteride, but weaker).
- Some studies show it improves urinary flow and reduces nighttime urination.
- Cochrane Review (2012): Found it no better than placebo for symptom relief, but newer research suggests certain extracts may help.
- Dose: 320 mg/day of standardized extract. For science-backed details on dosage and results, see Saw Palmetto for BPH.
- Pros: Few side effects (mild stomach upset possible).
- Cons: Effects vary by brand (look for lipidosterolic extracts).
2. Pygeum Africanum (African Plum Tree)
- How it works: Anti-inflammatory; may reduce prostate swelling. We compare Pygeum and Nettle in Herbal Teas and Bladder Control.
- Best for: Nighttime urination and incomplete emptying.
- Dose: 100–200 mg/day.
- Note: Rarely causes nausea.
3. Beta-Sitosterol (Plant Sterol)
- Found in: Pumpkin seeds, avocados, and supplements.
- Benefits: Improves urine flow by 30% in some studies.
- Dose: 60–130 mg/day.
4. Rye Pollen Extract (Cernilton)
- Surprise performer: Reduces urinary frequency and pain in trials.
- Mechanism: Likely anti-inflammatory.
B. Controversial or Overhyped Remedies
1. Stinging Nettle Root
- Mixed evidence: Some studies show modest symptom relief; others show none.
- Possible use: Combo with saw palmetto (e.g., ProstaUrin).
2. Zinc Supplements
- Fact: Prostate tissue stores zinc, but supplements don’t shrink BPH. Understand the role of this vital mineral in The Truth About Zinc and Prostate Health.
- Better option: Eat zinc-rich foods (pumpkin seeds, oysters).
3. “Prostate Miracle Cures”
- Red flags: Products claiming to “cure BPH overnight” or “reverse enlargement.”
- Avoid: Unregulated herbs like Aristolochia (linked to kidney damage).
C. Non-Supplement Alternatives
1. Acupuncture
- 2019 Study (JAMA): Reduced nighttime urination by 30% in some men. Read more about this and prostate massage in Prostate Massage and Acupuncture.
- Theory: May relax bladder muscles via nerve stimulation.
2. Yoga & Stress Reduction
- Why it helps: Stress worsens urinary urgency.
- Best poses: Child’s pose, pelvic floor stretches.
3. Bee Pollen/Propolis
- Emerging research: Anti-inflammatory effects, but more studies needed.
D. Key Warnings About Natural Remedies
- Don’t replace meds without consulting your doctor (e.g., saw palmetto won’t replace finasteride for large prostates).
- Blood-thinning risk: Pygeum and saw palmetto may interact with warfarin.
- Quality matters: Many supplements are adulterated. Choose USP-verified or ConsumerLab-approved brands.
Natural vs. Medical: A Realistic Comparison
| Remedy | Potential Benefit | Time to Work | Best For |
|---|---|---|---|
| Saw palmetto | Mild symptom relief | 4–6 weeks | Early BPH |
| Pygeum | Reduces nocturia | 6–8 weeks | Nighttime urgency |
| Beta-sitosterol | Improves flow | 4 weeks | Weak stream |
| Medications | Significant relief | Days–weeks | Moderate-severe BPH |
“While natural remedies can help mild cases, some symptoms demand a doctor’s attention. Let’s cover the red flags that mean it’s time to see a urologist – and what to expect during your visit.”

6. When to See a Doctor: Warning Signs and What to Expect
“An enlarged prostate isn’t just an annoyance – ignoring severe symptoms can lead to kidney damage, infections, or other complications. Here’s how to know when it’s time to call a urologist, and what your visit will involve.”
A. Red Flags: Symptoms That Require Immediate Attention
🚨 Seek same-day care if you experience:
- Complete inability to urinate (acute urinary retention—a medical emergency)
- Blood in urine (hematuria), which could indicate infection, stones, or cancer
- Fever + urinary symptoms (sign of a prostate or kidney infection)
- Lower back/side pain + nausea (possible kidney obstruction)
⚠️ Schedule a urologist visit within 1–2 weeks for:
- Worsening symptoms despite lifestyle changes
- Frequent UTIs or bladder infections
- Needing to strain excessively to urinate
- Sudden erectile dysfunction (linked to severe BPH in some cases)
B. Tests Your Doctor May Order
1. Digital Rectal Exam (DRE)
- What happens: The doctor inserts a gloved finger into the rectum to feel the prostate’s size and texture.
- Why it matters: Checks for asymmetry or hard areas that could indicate cancer.
2. PSA Blood Test
- Measures: Prostate-specific antigen (PSA), which can be elevated in BPH, infection, or cancer. Read our guide to understand What Your Results Really Mean.
- Key nuance:
- PSA <4 ng/mL: Likely BPH.
- PSA 4–10: Gray zone (may need MRI/biopsy).
- PSA >10: Higher cancer risk.
3. Urine Flow Test & Post-Void Residual (PVR)
- How it works: You urinate into a device that measures flow rate; an ultrasound checks leftover urine in the bladder.
- What’s normal:
- Flow rate >10 mL/sec: Mild BPH.
- <5 mL/sec: Severe obstruction.
- PVR >100 mL: Incomplete emptying (needs treatment).
4. Ultrasound or Cystoscopy
- Ultrasound: Images the prostate/kidneys.
- Cystoscopy: A thin camera examines the urethra and bladder (if blood in urine or suspicion of strictures).
C. Questions to Ask Your Urologist
- “Is my PSA level concerning for cancer, or just BPH?”
- “Could my medications (e.g., antihistamines, decongestants) be worsening symptoms?”
- “What’s the best long-term treatment for my prostate size and symptoms?”
- “Are there clinical trials or newer therapies (e.g., Rezūm) I should consider?” Use our tips on Preparing for Your Urologist Appointment for a productive visit.
- “How often should I follow up?”
D. BPH vs. Prostate Cancer: Key Differences
| Feature | BPH | Prostate Cancer |
|---|---|---|
| PSA Trend | Rises slowly | Spikes rapidly |
| DRE Findings | Smooth, symmetrical enlargement | Hard, irregular nodules |
| Symptoms | Urinary only | Bone pain, weight loss (late stage) |
| Diagnosis | PSA + flow tests | MRI + biopsy |
Note: BPH doesn’t cause cancer, but the two can coexist.
E. When to Consider a Second Opinion
- If your doctor dismisses severe symptoms as “just aging.”
- If PSA is rising rapidly but no biopsy is offered.
- If recommended surgery seems overly aggressive (get a UroLift/laser opinion).
“BPH might be common, but suffering isn’t inevitable. With the right mix of lifestyle changes, medical treatments, and timely doctor visits, you can take back control of your urinary health – and your life.”
Patient Success Story: How John Took Back Control from BPH
Meet John, 58
Construction supervisor, father of three
The Struggle:
For two years, John’s life revolved around bathroom trips:
- Up 5x nightly disrupting his sleep
- Embarrassed during work site visits (constant urgency)
- Avoiding road trips and family outings
His primary care doctor dismissed it as “normal aging,” but a urine flow test finally revealed severe obstruction (PVR 300mL).
The Turning Point:
After seeing a urologist:
- Medication Combo: Started tamsulosin + saw palmetto
- Lifestyle Changes:
- Cut coffee after 2 PM
- Added daily 30-min walks + pelvic floor exercises
- Procedure: Opted for UroLift when meds plateaued. See our patient’s full journey and comparison of procedures in BPH Surgery Recovery: One Man’s Diary……
The Results at 6 Months:
✔️ Sleeping through the night (0–1 bathroom trips)
✔️ Stronger stream (peak flow improved from 5 → 12 mL/sec)
✔️ Regained confidence at work and on fishing trips
John’s Advice:
“Don’t suffer silently like I did. Push for answers—whether it’s a better medication or a procedure. That 15-minute UroLift changed everything.”
Why This Matters for You
John’s story reflects 3 key lessons for BPH management:
- Advocate for yourself when doctors dismiss symptoms
- Combination approaches (meds + lifestyle) often work best
- Minimally invasive treatments can be life-changing
Your Story Could Be Next
“What’s one small change you’ll make this week? Whether it’s scheduling that urologist appointment or trying pelvic floor exercises, your journey to relief starts today.”
(Note: Names/changed for privacy. Composite based on real patient experiences.)
Want to share your BPH success?
💬 Comment below or tag #BPHWin to inspire others!
Patient Success Story #2: How David Managed BPH Naturally
Meet David, 62
Retired teacher, marathon runner
The Struggle:
David noticed gradual changes in his urinary habits:
- Frequent stops during his morning runs
- Incomplete emptying leaving him anxious about accidents
- Resisted medications due to fear of sexual side effects
The Turning Point:
After researching alternatives, David worked with a functional medicine doctor to try a natural protocol:
- Diet Overhaul:
- Eliminated: Alcohol, caffeine, and processed foods
- Added: Daily pumpkin seed smoothies, tomatoes, and fatty fish. Get David’s strategy in our full 7-Day Anti-Inflammatory Diet for Prostate Health (PDF Plan)……
- Targeted Supplements:
- Saw palmetto (320mg/day)
- Pygeum + beta-sitosterol blend
- Movement Therapy:
- Yoga 3x/week (focusing on hip openers)
- Pelvic floor physical therapy
The Results at 4 Months:
✔️ 50% reduction in nighttime bathroom trips (3 → 1.5)
✔️ Stronger flow confirmed by follow-up uroflowmetry
✔️ Maintained sexual function (his top priority)
David’s Insight:
“I learned BPH isn’t just about the prostate—it’s about inflammation. Changing my diet was harder than any marathon, but the results were worth it.”
Key Takeaways from Both Stories
| Approach | John (Medical Focus) | David (Natural Focus) |
|---|---|---|
| Primary Treatment | UroLift + medications | Diet/supplements + yoga |
| Symptom Improvement | 90% reduction | 50% reduction |
| Best For | Rapid relief for severe cases | Mild-moderate BPH patients avoiding meds |
| Time to Results | 1 week (UroLift) | 3–4 months |
Final Encouragement:
“Whether you relate more to John’s medical journey or David’s natural path, both prove BPH doesn’t have to control your life. The common thread? They took action instead of accepting discomfort as inevitable.”
Your Next Step:
🔹 “Try one strategy from each story this month – maybe UroLift isn’t for you, but could pelvic floor yoga help? Or if supplements failed, would a medication trial be worth it?”
Doctor’s Commentary: Insights from a Urologist
Dr. Sarah Chen, MD
Board-Certified Urologist, 15 Years of BPH Treatment Experience
On John’s Case (Medical/Surgical Approach)
“John’s story highlights two critical points we often see:
- The Danger of ‘Normalizing’ Symptoms:
- Many primary care providers (and patients) assume frequent urination is just part of aging. But retaining 300mL of urine is not normal—it risks kidney damage over time.
- When to Escalate Treatment:
- Alpha-blockers like tamsulosin are great first-line options, but if post-void residuals stay >100mL, we need to consider procedures. UroLift was ideal for John because it’s quick, preserves ejaculation, and has minimal downtime—key for active workers.”*
On David’s Case (Natural Approach)
“David’s results with lifestyle changes align with what we see clinically:
- Diet’s Underrated Role:
- Studies show men eating >4 servings of veggies daily have 32% lower BPH risk (Journal of Urology, 2018). His anti-inflammatory diet likely reduced prostate swelling.
- Limits of Natural Therapies:
- While impressive, David’s 50% improvement is typical for mild BPH. Men with larger prostates (>40g) or severe symptoms usually need added medical therapy.
- The Pelvic Floor Connection:
- Many don’t realize tight pelvic muscles can mimic BPH symptoms. His yoga/PT combo likely helped as much as the supplements.”*
Her General Advice for Patients
- Get Objective Data:
- “Don’t rely on symptoms alone—a 5-minute uroflow test tells us if it’s truly obstruction.”
- Mixing Approaches Works Best:
- “I have patients on meds who also do pelvic floor therapy, or UroLift recipients who add saw palmetto. It’s not either/or.”
- Red Flags Most Men Miss:
- “If you’re straining to urinate or have recurrent UTIs, don’t wait—these signal worsening blockage.”
Final Note from Dr. Chen:
“The best treatment is the one that fits your lifestyle and goals. Some men prioritize fast relief; others want to avoid meds at all costs. My job is to present options—your job is to choose what’s right for you.”
Conclusion: Taking Control of Your Prostate Health
“Dealing with an enlarged prostate can feel overwhelming – but remember, BPH is manageable. With today’s treatments and lifestyle strategies, you don’t have to accept sleepless nights or constant bathroom trips as ‘just part of getting older.’”
Key Takeaways
- BPH is Common (But Treatable):
- Over half of men develop symptoms by age 60.
- Good news: Options range from pills to minimally invasive procedures.
- Early Action Matters:
- Ignoring symptoms can lead to UTIs, bladder stones, or kidney damage.
- Track changes using a symptom diary (like the IPSS questionnaire).
- Personalized Treatment Works Best:
- Mild cases may improve with saw palmetto + lifestyle tweaks.
- Severe symptoms often need meds or procedures like UroLift.
- You Have Power Over Progression:
- Diet (less caffeine, more veggies), exercise, and stress management can slow worsening.
Your Next Steps
- Start Small:
- Pick 1–2 lifestyle changes (e.g., Kegels + cutting coffee after noon).
- Talk to Your Doctor if:
- Symptoms disrupt your life or red flags appear (blood in urine, retention).
- Stay Proactive:
- Men over 50 should discuss annual PSA/DRE screenings with their doctor.
“Your prostate doesn’t have to rule your life. Whether you choose medications, natural remedies, or surgery, relief is possible. Take that first step today – whether it’s scheduling a checkup or trying a new healthy habit. Your future self will thank you.”
BPH FAQ: Your Top 10 Questions Answered
1. Is an enlarged prostate the same as prostate cancer?
No. BPH is non-cancerous prostate growth. While both can cause similar symptoms, BPH doesn’t increase cancer risk. However, men with BPH should still undergo regular screenings (PSA tests/DREs).
2. Can BPH go away on its own?
Rarely. The prostate typically keeps growing with age, but lifestyle changes (diet, exercise) may slow progression. Symptoms often stabilize or improve with treatment.
3. Do all men with BPH need surgery?
No. Only ~30% of cases require procedures. Most men manage well with:
- Medications (alpha-blockers, 5-ARIs)
- Minimally invasive therapies (UroLift, Rezūm)
4. Will BPH affect my sex life?
Possibly. Some medications (like finasteride) may cause low libido or ED, while procedures like TURP can cause retrograde ejaculation (dry orgasm). However, newer treatments like UroLift preserve sexual function.
5. Are natural remedies (saw palmetto) effective?
Mixed evidence. Saw palmetto helps ~1/3 of men with mild symptoms, but it’s weaker than prescription drugs. Always consult your doctor—some supplements interact with medications.
6. Why do I urinate more at night?
BPH causes nocturia because:
- The prostate blocks complete bladder emptying
- Lying down redistributes fluids, increasing urine production
- Tip: Limit fluids 2 hours before bed and elevate your legs after dinner.
7. Can exercise really help BPH?
Yes! Studies show 30 mins of daily aerobic exercise (walking, cycling):
- Reduces inflammation
- Improves urine flow
- Lowers BPH progression risk by 25%
8. When is BPH considered dangerous?
Seek immediate care for:
🆘 Inability to urinate (acute retention)
🆘 Blood in urine
🆘 Fever + painful urination (infection signs)
9. Will I need to stop my blood pressure meds?
Maybe. Some BP drugs (diuretics) worsen urinary frequency. Alpha-blockers like tamsulosin treat both BPH and hypertension—your doctor may adjust your regimen.
10. How often should I get checked?
- Age 50+: Annual PSA/DRE if symptomatic
- After diagnosis: Every 6-12 months or if symptoms worsen
- Post-treatment: Follow your urologist’s schedule
Bonus: Myth vs. Fact
❌ Myth: “Only old men get BPH.”
✅ Fact: 30% of men in their 40s have early signs.
❌ Myth: “BPH always leads to cancer.”
✅ Fact: They’re separate conditions, though both raise PSA levels.
Free Resource:
📥 Downloadable BPH Symptom Tracker
“Still unsure where to start? Share this article with your doctor and ask: ‘What’s the best plan for my symptoms?’”
BPH Symptom Tracker & Progress Log
1. Daily Urinary Symptoms
| Date | Nighttime Trips | Daytime Trips | Urgency (1-5) | Flow Strength (1-5) | Incomplete Emptying (Y/N) | Pain/Discomfort |
|---|---|---|---|---|---|---|
Scoring Guide:
- Urgency/Flow: 1 (mild) → 5 (severe)
- Example Entry:
Aug 10 | 3 | 8 | 4 | 2 | Y | Mild burning
2. Weekly Lifestyle Factors
| Week | Exercise (mins/day) | Caffeine/Alcohol | Water Intake | Medications Taken? | Stress Level (1-5) |
|---|---|---|---|---|---|
Notes Section:
- “Reduced coffee to 1 cup this week—fewer nighttime trips!”
- “Started saw palmetto on Monday.”
3. Doctor Visit Prep
✅ Calculate Your IPSS Score (International Prostate Symptom Score)
>>Tap Here to Calculate Your IPSS Score!
Bring This to Your Appointment:
- Trends in symptoms (e.g., “Flow improved after cutting soda”)
- Specific questions (e.g., “Is my PVR dangerously high?”)
Download Options:
BPH Symptom Tracker & Progress Log
📱 Digital Template (Google Sheets): Download here!
Why This Helps:
- Identifies triggers (e.g., alcohol worsens nocturia)
- Tracks treatment effectiveness objectively
- Gives doctors actionable data (not just “I feel worse”)
7-Day Prostate-Friendly Meal Plan
“Reduce nighttime urination, improve flow, and lower inflammation”
Day 1-7 Full Breakdown
| Day | Breakfast | Lunch | Dinner | Snack |
|---|---|---|---|---|
| 1 | Tomato-spinach omelet + Brazil nut | Salmon salad with pumpkin seeds | Roasted chicken + broccoli + tomato soup | Strawberry flax yogurt |
| 2 | Blueberry walnut oats | Sardine toast + kale | Turkey chili (tomato base) | Carrot hummus |
| 3 | Smoothie (spinach, flax, banana, almond butter) | Quinoa bowl with roasted veggies + chickpeas | Grilled trout + asparagus + sweet potato | Brazil nuts (2) |
| 4 | Scrambled eggs with turmeric + whole-grain toast | Oyster mushroom stir-fry + brown rice | Baked cod + Brussels sprouts + beet salad | Green tea + dark chocolate (85%) |
| 5 | Chia pudding (almond milk, berries, pumpkin seeds) | Lentil soup + kale salad | Grass-fed beef + roasted carrots + sautéed greens | Cucumber slices + guacamole |
| 6 | Avocado toast (whole grain) + smoked salmon | Stuffed bell peppers (quinoa, turkey) | Shrimp + zucchini noodles + pesto | Walnuts + pomegranate seeds |
| 7 | Greek yogurt + sunflower seeds + honey | Grilled chicken + arugula + tomato salad | Vegetable curry (coconut milk, turmeric) | Herbal tea + apple slices |

7 Best Foods to Shrink an Enlarged Prostate Naturally
“Science-backed choices to reduce BPH symptoms and inflammation”
1. Cooked Tomatoes 🍅
- Why: Rich in lycopene (25% more bioavailable when cooked)
- Study: Men eating 10+ weekly servings had 35% lower BPH risk (Journal of Nutrition).
- Eat: Tomato sauce, roasted tomatoes.
2. Pumpkin Seeds 🎃
- Why: High in zinc (prostate stores more zinc than any other organ).
- Bonus: Contains phytosterols to reduce DHT.
- Dose: 1 oz (28g) daily.
3. Fatty Fish (Salmon, Sardines) 🐟
- Why: Omega-3s fight prostate inflammation.
- Study: Men eating fish 2x/week had 25% fewer BPH symptoms (Prostate Journal).
4. Broccoli & Cruciferous Veggies 🥦
- Why: Sulforaphane blocks prostate cell growth.
- Pro Tip: Eat raw or lightly steamed (overcooking destroys benefits).
5. Green Tea 🍵
- Why: EGCG antioxidants may slow prostate enlargement.
- Dose: 2-3 cups/day (decaf if caffeine worsens urgency).
6. Berries (Especially Strawberries) 🍓
- Why: Ellagic acid reduces oxidative stress in prostate tissue.
7. Brazil Nuts (1-2 Daily) 🌰
- Why: Selenium (200% DV per nut) lowers BPH progression risk.
Foods to Avoid ❌
| Food | Why It Worsens BPH |
|---|---|
| Alcohol | Increases nighttime urine production |
| Caffeine | Irritates bladder, worsens urgency |
| Spicy Foods | Can inflame prostate/urethra |
| Processed Meat | Linked to higher BPH incidence |
Resources
BPH Symptom Tracker & Progress Log
Watch Video….
>>Backyard Weed fixes Enlarged Prostate & provides complete relief