The Unexpected Link Between Your Gut and Your Lungs
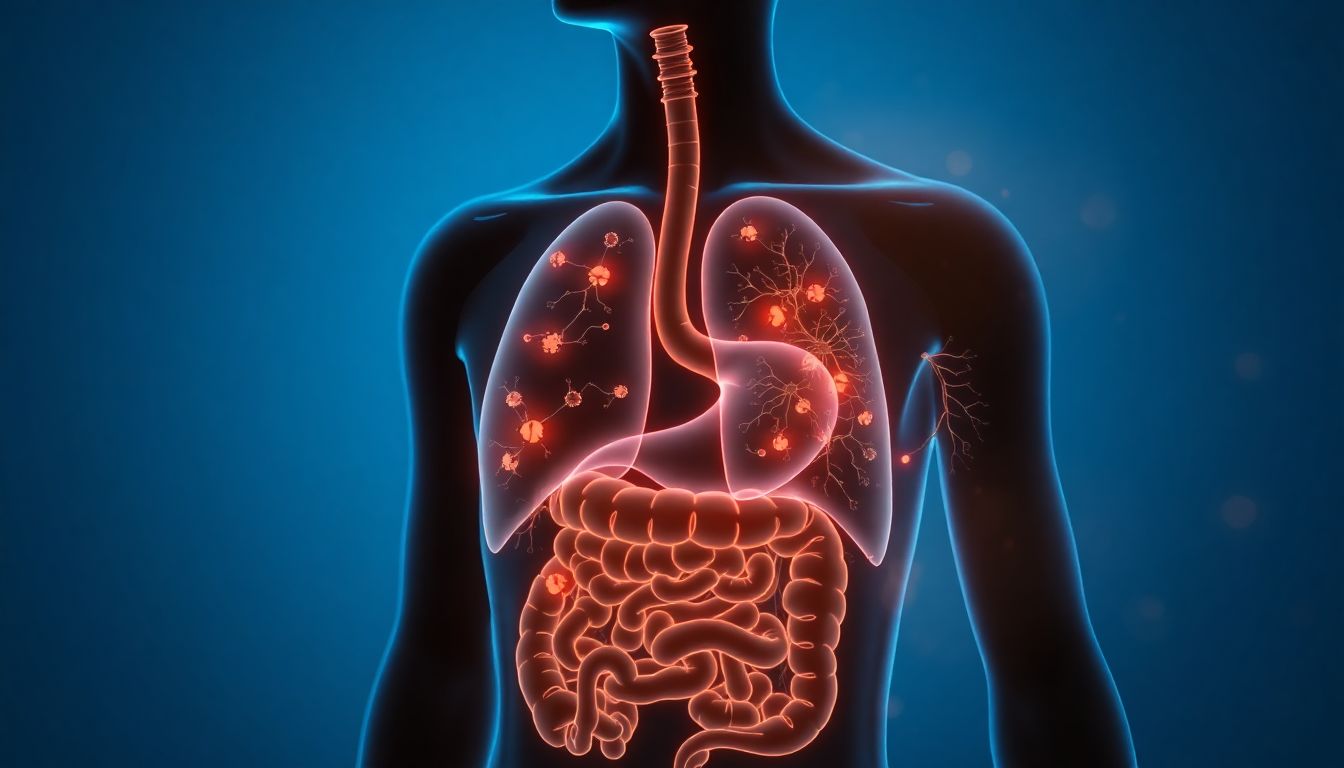
What if I told you that the key to solving your chronic cough, wheezing, or shortness of breath might not be in your lungs at all—but in your gut?
It sounds unbelievable, but groundbreaking research is revealing that your digestive system and respiratory system are in constant communication. That persistent chest tightness or nagging cough could actually be a message from your gut saying, “I need help!”
Meet Sarah, a 42-year-old teacher who struggled with asthma for years. “I was using my inhaler multiple times daily, but still woke up gasping,” she shares. “Then my doctor suggested addressing my digestive issues. Within three weeks of healing my gut, my breathing improved more than it had in a decade of asthma treatments.”
Sarah’s story isn’t unique. The gut-lung axis—the biochemical highway connecting your digestive and respiratory systems—might be the missing piece in your breathing puzzle.
The Science Behind the Gut-Lung Axis: Your Body’s Hidden Communication Network
The Shared Immune System
Your gut and lungs develop from the same embryonic tissue and remain intimately connected throughout your life. They share:
- 70% of your immune system resides in gut-associated lymphoid tissue (GALT)
- Identical mucosal lining that responds to similar triggers
- Direct neural pathways through the vagus nerve
- Common inflammatory responses to threats
The Inflammation Highway
When your gut becomes inflamed (from poor diet, stress, or toxins), it doesn’t stay contained. Inflammatory cytokines travel through your bloodstream, reaching your lungs and triggering:
- Bronchial constriction (airway tightening)
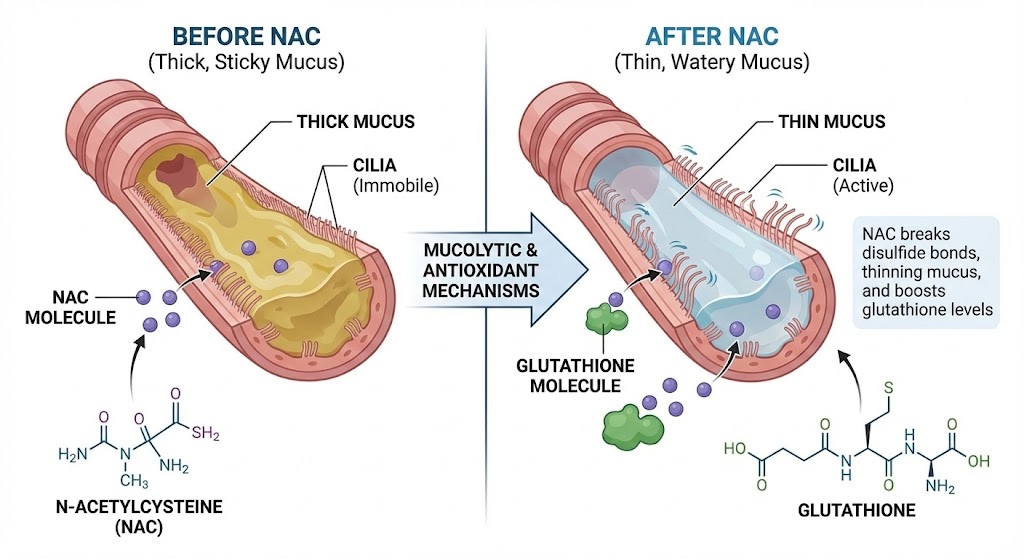
- Increased mucus production
- Heightened sensitivity to allergens
- Reduced lung function
“The gut is often the first responder to environmental threats, and the lungs pay the price when gut health suffers.” — Dr. Michael Ruscio, Digestive Health Expert
Leaky Gut: The Hidden Trigger Behind Respiratory Inflammation
What Is Leaky Gut?
Intestinal permeability (leaky gut) occurs when the tight junctions between cells in your intestinal lining weaken, allowing undigested food particles, toxins, and bacteria to enter your bloodstream.
The Domino Effect on Your Lungs
When these foreign particles escape your gut, your immune system sounds the alarm, creating systemic inflammation that particularly affects your lungs:
- Immune activation throughout your body
- Inflammatory cytokines target lung tissue
- Bronchial hyperresponsiveness develops
- Mucus production increases as a defense mechanism
Research shows that 73% of asthma patients have increased intestinal permeability, compared to 15% of healthy controls.
Your Gut Microbiome: The Army Protecting Your Lungs
The Good Bacteria Balance
Your gut houses trillions of bacteria that directly influence lung health through:
- Short-chain fatty acid production (butyrate, acetate, propionate)
- Immune system regulation
- Inflammation control
- Pathogen protection
The Asthma-Microbiome Connection
Studies reveal striking differences in gut bacteria between healthy individuals and those with respiratory conditions:
- Asthma patients typically have lower diversity of gut bacteria
- Reduced Bifidobacterium and Lactobacillus levels
- Higher inflammatory bacteria strains
- Imbalanced firmicutes-to-bacteroidetes ratio
The 3 Key Diet Shifts to Support Your Gut-Lung Axis
1. Increase Fiber & Prebiotics: Feed Your Good Bacteria
Best Foods:
- Jerusalem artichokes (the ultimate prebiotic)
- Garlic and onions (rich in inulin)
- Asparagus and leeks
- Green bananas and plantains
- Oats and barley
Why it works: Prebiotic fibers feed beneficial bacteria that produce anti-inflammatory compounds protecting your lungs.
2. Eat Fermented Foods: Add Good Bacteria Daily
Best Foods:
- Sauerkraut (unpasteurized)
- Kimchi (Korean fermented vegetables)
- Kombucha (fermented tea)
- Kefir (fermented milk drink)
- Miso (fermented soybean paste)
Start small: Begin with 1 tablespoon daily and gradually increase to avoid digestive discomfort.
3. Reduce Inflammatory Foods: Calm the System
Foods to minimize:
- Refined sugars and high-fructose corn syrup
- Processed vegetable oils (soybean, corn, canola)
- Industrial seed oils
- Processed meats with nitrates
- Excessive alcohol
Pro tip: Notice how you feel 2-3 hours after eating these foods. Many people report increased mucus production and breathing difficulties.
Should You Take a Probiotic? Evidence-Based Guidance
The Research-Backed Strains
Specific probiotic strains show promise for respiratory health:
- Lactobacillus rhamnosus GG: Reduces respiratory infection frequency
- Bifidobacterium lactis: Improves lung function in allergic asthma
- Lactobacillus casei: Decreases cold and flu duration
- Combination strains: Most effective for comprehensive support
When Probiotics Help Most
Consider probiotics if you:
- Take antibiotics frequently
- Have diagnosed digestive issues
- Experience frequent respiratory infections
- Have food sensitivities or allergies
“Look for products containing multiple strains with at least 10-20 billion CFUs for respiratory benefits.” — Dr. Heather Moday, Immunologist
Real Results: Maria’s Gut-Lung Transformation
Maria, 58, had battled COPD for 12 years. “I was constantly short of breath and needed steroid inhalers daily,” she recalls. “My doctor mentioned the gut connection almost as an afterthought.”
She implemented the three diet shifts:
- Added sauerkraut to her lunch daily
- Increased vegetable diversity to 8+ types weekly
- Eliminated processed sugars
“Within six weeks, I was using my rescue inhaler 80% less. My pulmonologist was shocked at my improved lung function tests. Healing my gut literally helped me breathe easier.”
Conclusion: Your Path to Better Breathing Starts in Your Gut
The evidence is clear: you cannot separate respiratory health from digestive health. Your gut and lungs are partners in your body’s defense system, constantly communicating and influencing each other’s function.
Your 3-Step Action Plan:
- Start with one change—add one fermented food or increase vegetable variety
- Notice the connections—keep a simple journal of diet and breathing patterns
- Be patient—gut healing takes 4-8 weeks to show significant respiratory benefits
The next time you reach for your inhaler or struggle to take a deep breath, remember: the solution might be closer than you think. Your kitchen—not just your medicine cabinet—could hold the key to lasting respiratory relief.
Ready to explore more natural approaches to lung health? Discover comprehensive strategies in our Ultimate Guide to Clearing Mucus & Restoring Lung Health Naturally.