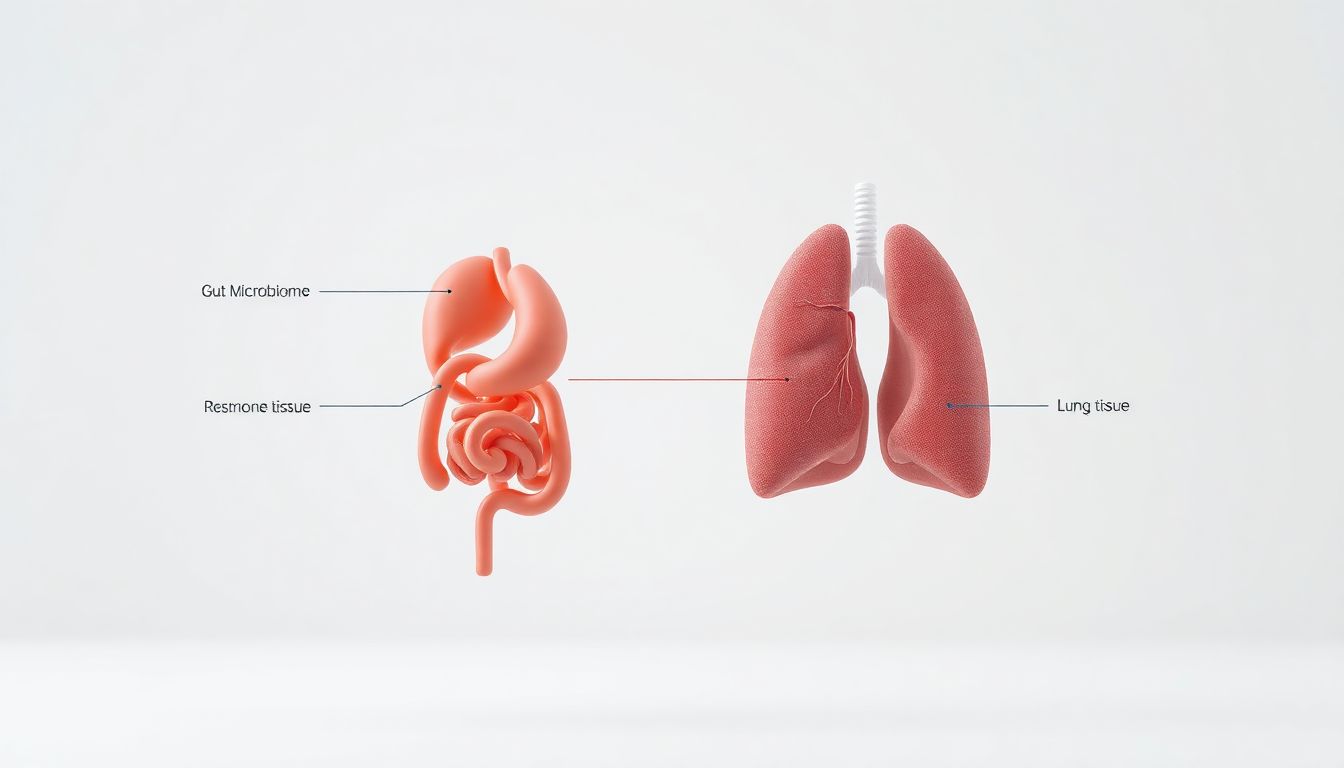
What if the secret to better breathing wasn’t in your lungs, but in your gut? Emerging research is revealing a powerful bidirectional relationship between your digestive system and respiratory health—a link known as the gut-lung axis.
This connection explains why digestive issues often coincide with breathing problems, and how optimizing your gut health could be a missing piece in your lung health strategy.
What is the Gut-Lung Axis?
The gut-lung axis refers to the complex communication network between your gastrointestinal tract and your respiratory system. This connection operates through several key pathways:
- Shared Microbiome: Both systems have their own microbial ecosystems that communicate and influence each other.
- Immune System Cross-Talk: 70-80% of your immune cells reside in your gut, directly impacting how your lungs respond to pathogens and inflammation.
- Inflammatory Pathways: Gut inflammation can trigger systemic inflammation that affects lung tissue.
- Vagus Nerve: This “information superhighway” carries signals between your gut and lungs.
“When the gut microbiome is disrupted, it can lead to increased inflammation throughout the body, including the airways,” explains Dr. Michael Chen, a respiratory researcher. “This is particularly relevant for conditions like asthma and COPD.”
Scientific Evidence: The Research Behind the Connection
The Microbiome’s Role in Respiratory Health
A 2023 meta-analysis in Nature Communications found that individuals with respiratory conditions consistently showed reduced gut microbiome diversity compared to healthy controls. Specifically:
- Asthma: Children with asthma showed significantly different gut bacteria composition, with lower levels of beneficial Bifidobacterium and Lactobacillus species.
- COPD: Patients often have gut dysbiosis that correlates with more frequent exacerbations and worse lung function.
- COVID-19: Research found that gut microbiome composition predicted disease severity, with healthier microbiomes associated with milder symptoms.
Leaky Gut and Lung Inflammation
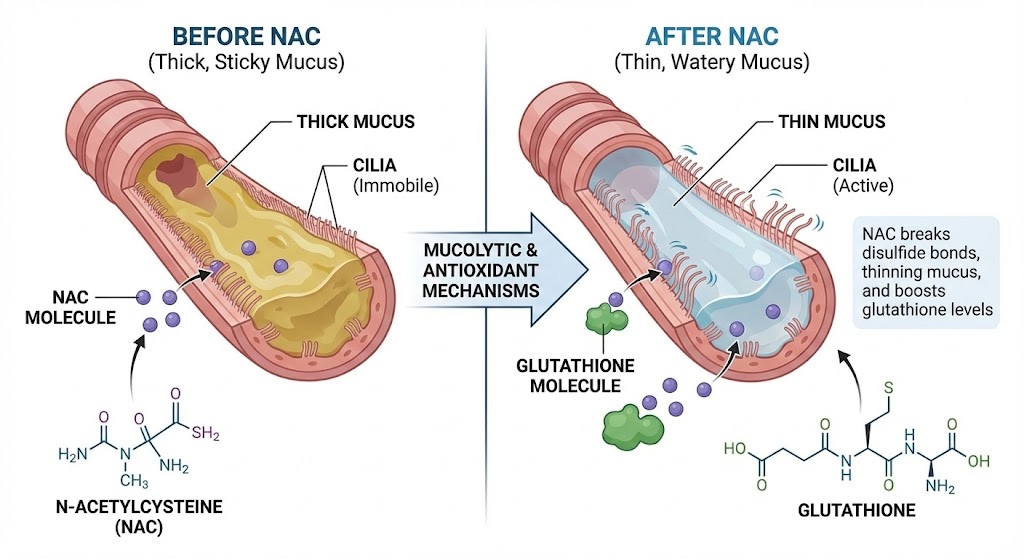
When the gut lining becomes permeable (“leaky gut”), toxins and undigested food particles enter the bloodstream, triggering widespread inflammation. This systemic inflammation can:
- Worsen airway hyperresponsiveness
- Increase mucus production
- Reduce the lungs’ ability to fight infections
5 Ways Your Gut Health Impacts Your Breathing
1. Immune System Regulation
Your gut microbiome trains your immune system to distinguish between harmless substances and genuine threats. An imbalanced gut can lead to overactive immune responses in the lungs, contributing to allergic asthma and excessive inflammation.
2. Short-Chain Fatty Acid Production
Beneficial gut bacteria produce short-chain fatty acids (SCFAs) like butyrate when they ferment dietary fiber. These SCFAs:
- Reduce airway inflammation
- Strengthen the lung epithelial barrier
- Modulate immune responses to respiratory viruses
3. Microbial Metabolite Exchange
Gut bacteria produce metabolites that enter the bloodstream and directly affect lung function. Meanwhile, lung inflammation can alter gut permeability and microbiome composition, creating a feedback loop.
4. Nutrient Absorption for Lung Tissue
A healthy gut is essential for absorbing key nutrients that support lung health, including:
- Vitamin D (crucial for immune function)
- Magnesium (helps relax bronchial muscles)
- Omega-3 fatty acids (reduce inflammation)
5. Stress Response Coordination
The gut-brain-lung connection means that stress-induced gut changes can directly impact breathing patterns and airway function.
Practical Steps to Support the Gut-Lung Axis
Dietary Strategies for Dual Health
- Increase Fermented Foods: Yogurt, kefir, kimchi, and sauerkraut introduce beneficial bacteria.
- Eat Diverse Fiber: Aim for 30+ different plant foods weekly to feed various gut microbes.
- Include Polyphenol-Rich Foods: Berries, green tea, dark chocolate, and nuts support good bacteria.
- Consider Bone Broth: The collagen and gelatin may help repair gut lining.
Many of these foods overlap with our recommendations for lung-cleansing foods, creating a powerful synergy.
Lifestyle Factors
- Manage Stress: Chronic stress damages gut lining and worsens inflammation.
- Avoid Unnecessary Antibiotics: They devastate gut microbiome diversity.
- Get Quality Sleep: Poor sleep disrupts gut health and increases inflammation.
- Exercise Regularly: Moderate activity supports microbiome diversity.
Targeted Supplement Support
While a healthy diet is foundational, certain supplements can provide additional support:
- Probiotics: Specific strains like Lactobacillus rhamnosus and Bifidobacterium breve show promise for respiratory health.
- Vitamin D: Essential for both gut integrity and immune function in the lungs.
- Omega-3s: Powerful anti-inflammatory support for both systems.
For comprehensive respiratory support, some people find that combining gut health strategies with targeted lung supplements like Breathe Drops provides the most complete approach.
Case Study: Integrating Gut and Lung Health
Background: Sarah, 42, with adult-onset asthma and IBS symptoms.
4-Month Protocol:
- Months 1-2: Focused on gut healing with probiotics, glutamine, and an anti-inflammatory diet.
- Months 3-4: Added daily breathing exercises and maintained gut protocol.
Results:
- Asthma inhaler use reduced by 70%
- Morning peak flow readings improved by 15%
- Digestive symptoms resolved by 90%
- Reported better energy and sleep quality
“The gut-focused approach was the missing piece my pulmonologist never mentioned,” Sarah reported.
✅ FAQ
1. Can improving my gut health really help my asthma?
Yes, multiple studies show that optimizing gut microbiome diversity can reduce asthma severity, particularly in cases with allergic components. The gut’s role in immune regulation directly impacts airway inflammation.
2. What are the signs that my gut health might be affecting my lungs?
Common signs include: asthma that worsens with digestive issues, increased respiratory infections, developing respiratory symptoms after food sensitivities, and conditions like IBS coinciding with breathing problems.
3. How long does it take to see improvements in breathing from gut healing?
Most people notice some improvement in 4-8 weeks, but significant changes to the microbiome and immune system can take 3-6 months of consistent effort. This is similar to the timeline for seeing results from lung detox supplements.
4. Are probiotics safe for people with COPD?
Generally yes, but consult your doctor first, especially if you have severe COPD or are immunocompromised. Some studies suggest specific probiotic strains may reduce exacerbation frequency.
5. Can gut health affect sleep apnea?
Yes, research shows connections between gut microbiome composition and sleep apnea severity, likely through inflammatory pathways. Improving gut health may help reduce apnea episodes.
6. What’s the best probiotic for lung health?
Look for strains with respiratory research, including Lactobacillus rhamnosus GG, Bifidobacterium lactis, and Lactobacillus casei. Multi-strain probiotics are often more effective than single strains.
7. Can antibiotics for respiratory infections damage gut health?
Yes, antibiotics significantly disrupt gut microbiome diversity. If you need antibiotics, take high-quality probiotics 2-3 hours apart from antibiotic doses and continue for several weeks after finishing the course.
8. How does stress affect the gut-lung connection?
Stress increases gut permeability and inflammation, which can trigger or worsen asthma and COPD symptoms. Stress management techniques like the 4-7-8 breathing method can help both systems.
9. Are there specific foods that harm both gut and lung health?
Highly processed foods, excessive sugar, and foods you’re sensitive to (common culprits include dairy and gluten for some people) can increase inflammation in both systems.
10. Should I get my gut microbiome tested?
While not essential, testing can identify specific imbalances and guide targeted interventions. However, most people benefit from the general gut-health strategies outlined above regardless of test results.
Still Have Questions? We Have Answers.
Lung health is complex. If you’re wondering “What about…?” or “What’s next for me?”, you’re not alone. Our Resource Hub is built to be your **first stop for trustworthy, in-depth answers** on every aspect of respiratory wellness.
- Condition-Specific Guides (COPD, Asthma, Post-COVID)
- Step-by-Step Detox & Recovery Plans
- Science-Backed Natural & Conventional Strategies