If you find yourself reaching for your inhaler every time pollen season hits, you’re experiencing what’s known as the allergy-asthma connection—a frustrating cycle where allergic reactions trigger asthma symptoms, creating a cascade of respiratory distress. Understanding and addressing this overlap is key to breaking free from seasonal suffering.
This evidence-based guide explores the biological link between allergies and asthma and provides natural strategies to manage both conditions simultaneously.
Understanding the Allergy-Asthma Connection
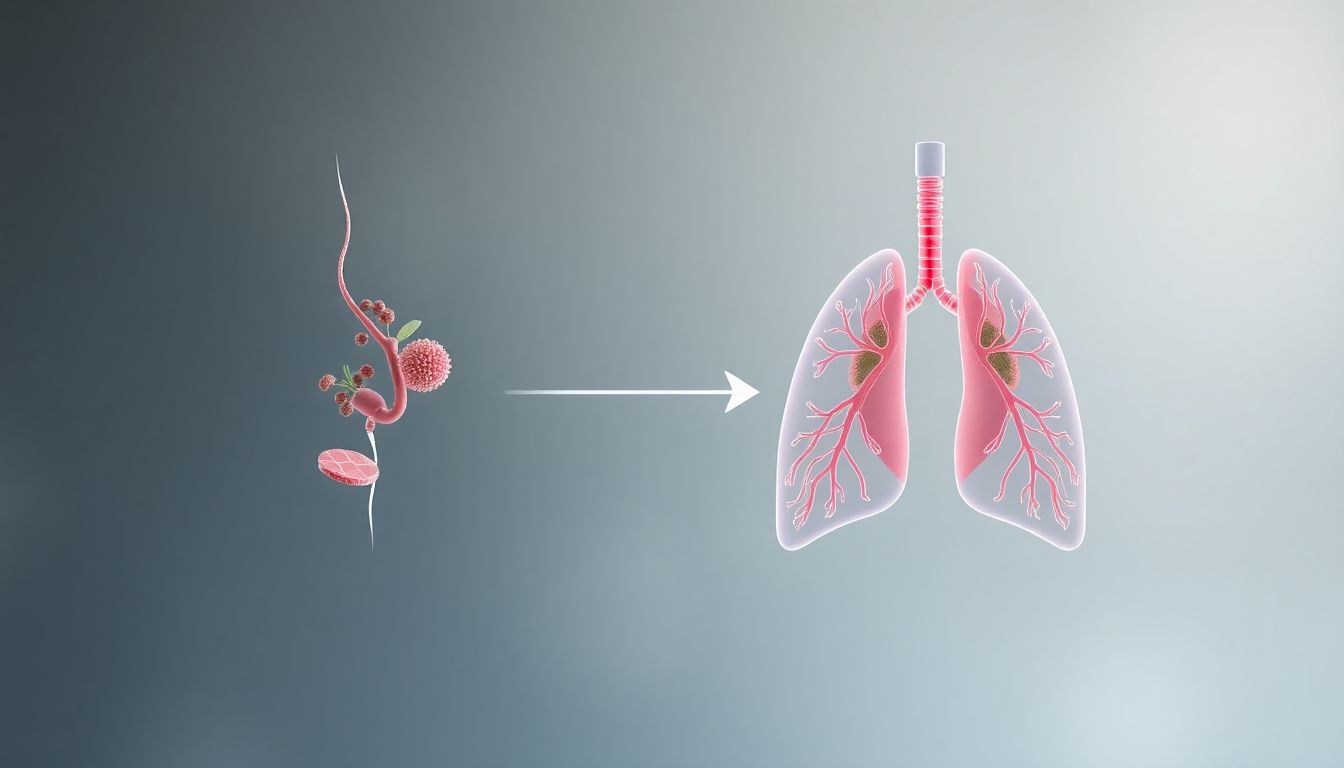
The Unified Airway Theory
Medical research now recognizes that the upper and lower airways function as a single unit. What affects your nose and sinuses inevitably impacts your lungs through several mechanisms:
- Inflammatory Cascade: Allergens trigger immune responses that create system-wide inflammation
- Nasal-Bronchial Reflex: Irritated nasal passages send signals that constrict bronchial tubes
- Post-Nasal Drip: Inflammatory mediators drip into lungs, worsening airway reactivity
“Approximately 80% of people with asthma also have allergic rhinitis, and treating allergies often significantly improves asthma control,” explains Dr. Sarah Chen, an allergist and immunologist.
The Vicious Cycle: How Allergies Trigger Asthma
Step 1: Allergen Exposure
Pollen, mold, dust mites, or pet dander enter your respiratory system
Step 2: Immune System Activation
Mast cells release histamine and other inflammatory compounds
Step 3: Upper Airway Inflammation
Nasal passages swell, leading to congestion and post-nasal drip
Step 4: Lower Airway Effects
Inflammatory mediators reach lungs, causing:
- Bronchial constriction
- Increased mucus production
- Airway hyperresponsiveness
Step 5: Asthma Symptoms
- Wheezing
- Shortness of breath
- Chest tightness
- Coughing
Natural Strategies to Break the Cycle
1. Identify and Reduce Triggers
Common Overlap Triggers:
- Pollen (tree, grass, weed)
- Mold spores (indoor and outdoor)
- Dust mites in bedding and upholstery
- Pet dander from cats, dogs, rodents
- Cockroach allergens in urban environments
Reduction Strategies:
- HEPA air purifiers in bedroom and main living areas
- Allergen-proof bedding covers for pillows and mattresses
- Regular vacuuming with HEPA-filter machines
- Humidity control (30-50% to discourage dust mites and mold)
2. Dietary Anti-Inflammatory Support
Foods to Emphasize:
- Omega-3 rich foods: Wild salmon, flaxseeds, walnuts (reduce inflammation)
- Quercetin sources: Apples, onions, capers, citrus (natural antihistamine)
- Vitamin C foods: Bell peppers, broccoli, strawberries (reduces histamine)
- Local raw honey: Small daily amounts may help desensitize to local pollen
Foods to Limit:
- Dairy products (can increase mucus production in some people)
- Highly processed foods (promote systemic inflammation)
- Food additives and preservatives (may trigger reactions)
3. Nasal and Sinus Care
Daily Saline Rinse:
- Helps flush allergens from nasal passages
- Reduces post-nasal drip reaching lungs
- Improves overall airway health
Steam Inhalation:
- With eucalyptus or tea tree oil (if not allergic)
- Helps open nasal passages and soothe airways
- Particularly helpful during high-pollen seasons
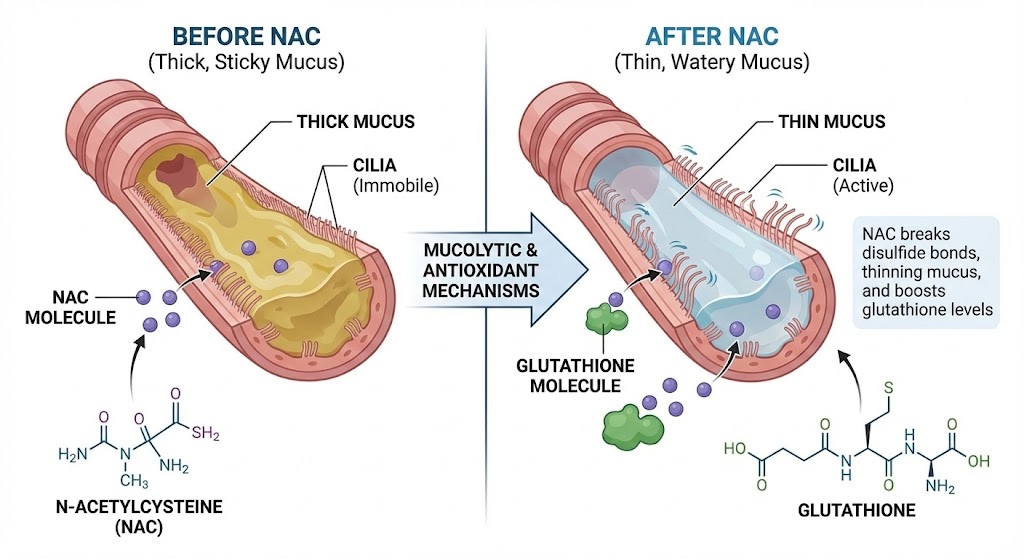
4. Targeted Supplement Support
Butterbur Extract:
- Clinical evidence: As effective as some antihistamines for allergic rhinitis
- Mechanism: Reduces inflammation and allergic response
- Dosage: 50-75 mg twice daily during allergy season
Quercetin with Bromelain:
- Natural antihistamine properties
- Stabilizes mast cells to prevent histamine release
- Bromelain enhances absorption and reduces mucus
- Mullein leaf soothes irritated respiratory tissues
- Thyme provides natural antimicrobial support
- Oregano oil helps combat inflammatory responses
Stinging Nettle:
- Natural anti-inflammatory for allergic responses
- Freeze-dried form most effective
- Dosage: 300-600 mg daily during symptom periods
5. Breathing Retraining
Buteyko Breathing Method:
- Helps reduce airway hyperresponsiveness
- Teaches nasal breathing to filter and warm air
- Can reduce both allergy and asthma symptoms
- Strengthens respiratory muscles
- Improves oxygen exchange
- Reduces stress that can worsen both conditions
Seasonal Preparation Protocol
4-6 Weeks Before Allergy Season
- Begin preventive supplements (quercetin, stinging nettle)
- Start local raw honey (1 teaspoon daily)
- Optimize indoor air quality with HEPA filters
- Review and update asthma management plan
During High-Pollen Seasons
- Keep windows closed during high pollen counts
- Shower before bed to remove pollen from hair and skin
- Change clothes after being outdoors
- Use saline nasal rinse morning and evening
- Monitor pollen forecasts and plan activities accordingly
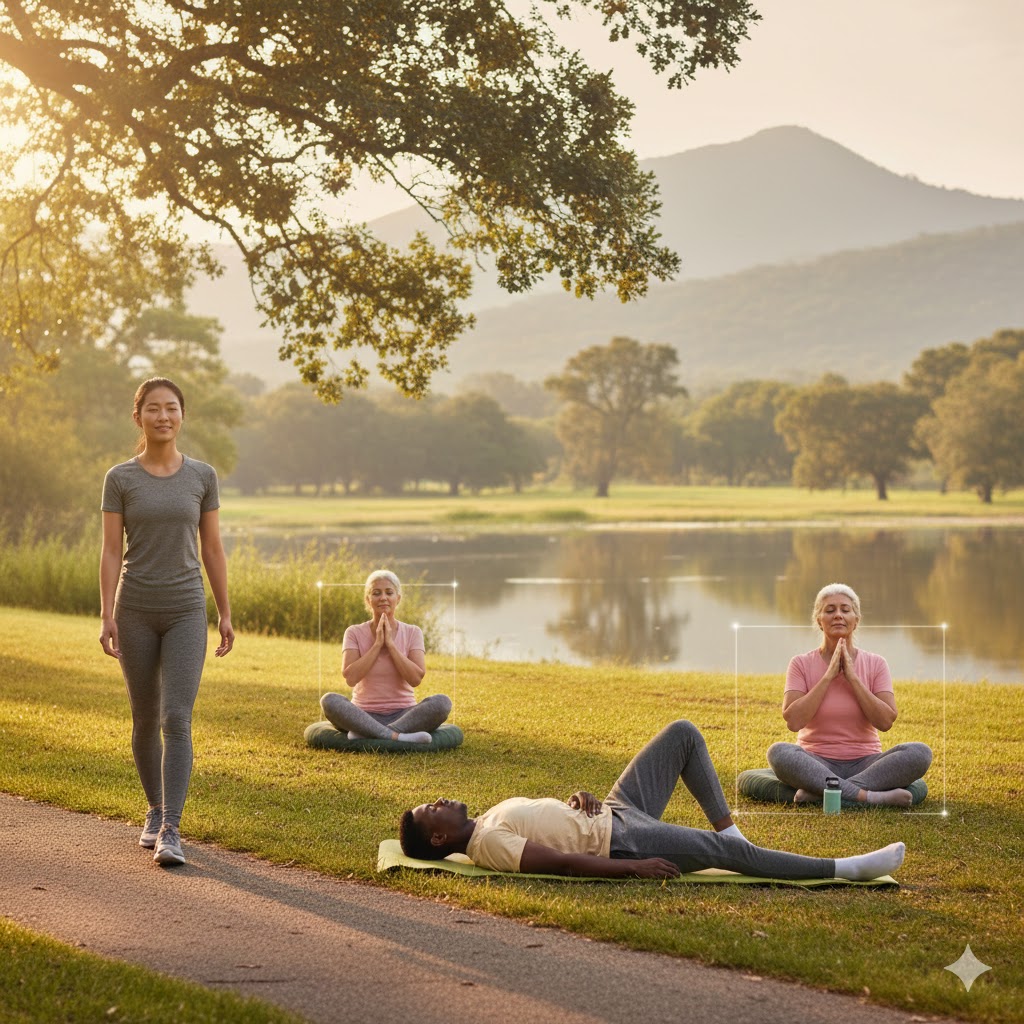
Lifestyle Factors That Reduce Reactivity
Stress Management
- Chronic stress increases inflammatory responses
- Cortisol dysregulation worsens both allergies and asthma
- Practice mindfulness or meditation to modulate immune function
Sleep Optimization
- Poor sleep increases inflammatory markers
- Aim for 7-9 hours of quality sleep nightly
- Elevate head slightly to reduce nighttime post-nasal drip
Regular Moderate Exercise
- Improves lung function and reduces airway inflammation
- Avoid outdoor exercise during high pollen counts
- Indoor alternatives during peak allergy seasons
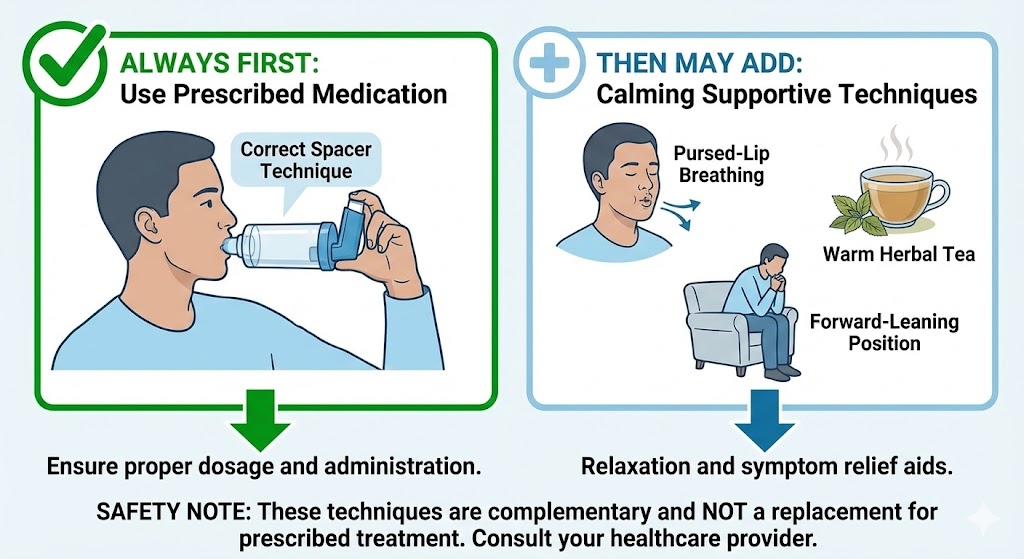
When Natural Approaches Need Support
Integrating Conventional Treatments
While natural strategies form a strong foundation, some situations require medical support:
Allergy Medications That May Help:
- Nasal corticosteroids (reduce inflammation with minimal systemic effects)
- Antihistamines (for breakthrough symptoms during high exposure)
- Leukotriene modifiers (address the inflammatory pathway common to both conditions)
Immunotherapy Considerations:
- Allergy shots or sublingual tablets
- Can modify the underlying immune response
- Most effective for clearly identified triggers
Tracking Your Progress
Keep a symptom journal to identify patterns:
- Daily pollen counts and weather conditions
- Symptom severity (nasal and respiratory)
- Medication and supplement use
- Diet and environmental exposures
- Stress levels and sleep quality
Special Considerations
For Children with Both Conditions
- More aggressive trigger avoidance may be necessary
- Monitor growth as both conditions and medications can affect it
- School environment management requires planning with staff
For Older Adults
- Medication interactions become more concerning
- Co-existing conditions like COPD may complicate management
- Immune system changes may alter typical response patterns
✅ FAQ
1. Can treating my allergies really improve my asthma?
Yes, comprehensively. Studies show that effectively managing allergic rhinitis can reduce asthma symptoms by 40-50% and decrease the need for rescue inhalers. The inflammatory pathways are shared, so addressing one condition helps the other.
2. What’s the difference between allergic asthma and regular asthma?
Allergic asthma is triggered specifically by allergens and involves IgE antibody responses, while non-allergic asthma may be triggered by exercise, cold air, infections, or irritants. However, most people with asthma have mixed triggers.
3. How long does it take for natural approaches to work?
Some strategies like saline rinses and avoiding triggers provide immediate relief. Dietary changes and supplements typically show effects within 2-4 weeks, with maximum benefit after 2-3 months of consistent use.
4. Are there specific tests to confirm the allergy-asthma connection?
Yes, allergy testing (skin prick or blood tests for specific IgE) can identify triggers. Pulmonary function tests can confirm asthma diagnosis and severity. Seeing both an allergist and pulmonologist provides the most comprehensive assessment.
5. Can I outgrow the allergy-asthma connection?
Some children outgrow both conditions, but adults typically experience fluctuating severity rather than complete resolution. However, effective management can make symptoms minimal to nonexistent for extended periods.
6. What are the most common mistake people make managing both conditions?
Treating asthma and allergies as separate issues rather than interconnected conditions. Also, stopping medications when feeling better rather than maintaining preventive strategies.
7. How does stress affect the allergy-asthma cycle?
Stress increases cortisol and inflammatory markers, making both allergic responses and airway reactivity worse. Stress management is a crucial, often overlooked component of comprehensive care.
8. Are there any risks to using natural approaches?
Most are very safe, but herb-drug interactions are possible. Butterbur should be PA-free (pyrrolizidine alkaloids removed). Always discuss new supplements with your healthcare provider, especially if taking medications.
9. Can improving gut health help with allergies and asthma?
Emerging research on the gut-lung axis suggests that a healthy microbiome can modulate immune responses and reduce inflammatory conditions throughout the body, including allergic asthma.
10. When should I see a specialist for the allergy-asthma overlap?
Consider specialist referral if: symptoms interfere with daily activities despite treatment, you require frequent rescue medication, symptoms wake you at night, or you’ve experienced a severe asthma attack requiring emergency care.
Still Have Questions? We Have Answers.
Lung health is complex. If you’re wondering “What about…?” or “What’s next for me?”, you’re not alone. Our Resource Hub is built to be your **first stop for trustworthy, in-depth answers** on every aspect of respiratory wellness.
- Condition-Specific Guides (COPD, Asthma, Post-COVID)
- Step-by-Step Detox & Recovery Plans
- Science-Backed Natural & Conventional Strategies