1. Introduction: Why Metabolic Health Is the Foundation of Everything
Blood sugar is not just a concern for people with diabetes. It is the core energy system of the human body, influencing how you feel, think, sleep, store fat, and age.
When blood sugar is stable, energy is steady, cravings are manageable, and focus is sharp.
When it is unstable, the body enters a destructive cycle of spikes and crashes — often without obvious warning signs at first.
Modern diets, chronic stress, ultra-processed foods, poor sleep, and sedentary lifestyles have created what many experts now call the metabolic rollercoaster. Blood sugar rises rapidly after meals, crashes soon after, and over time forces the body to produce more and more insulin just to keep up.
This guide exists to change that trajectory.
In this comprehensive resource, you will learn:
- How blood sugar actually works inside the body
- What “normal” levels really look like
- How nutrition, movement, stress, and sleep interact with glucose
- Which natural strategies have real scientific backing
- How to build a sustainable plan that works long-term, not just for a week
This is natural blood sugar management, explained clearly and practically.
2. Blood Sugar 101: How Your Body Manages Energy
The Insulin–Glucose Relationship (Simplified)
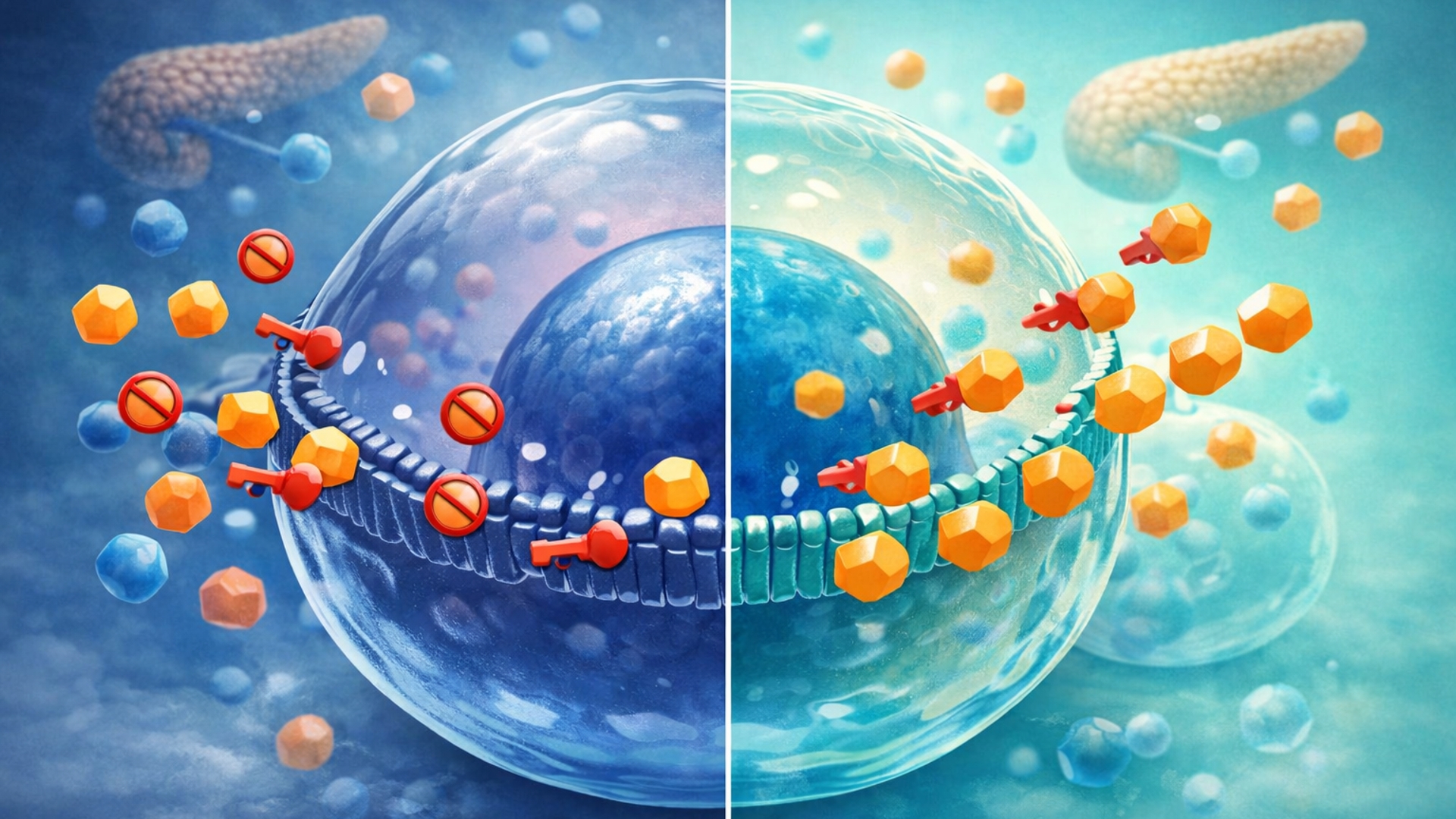
When you eat carbohydrates, they are broken down into glucose, which enters your bloodstream. Glucose is fuel — but it must be transported into cells to be used.
That job belongs to insulin, a hormone produced by the pancreas.
Think of insulin as a key:
- Glucose is the fuel outside the cell
- Insulin unlocks the door so glucose can enter
When this system works well, blood sugar rises modestly after meals and returns to baseline within a few hours.
What Is Insulin Resistance?
Over time, repeated glucose spikes cause cells to become less responsive to insulin. The pancreas compensates by releasing more insulin, which temporarily works — until it doesn’t.
This condition is known as insulin resistance, and it is a major driver of:
- Prediabetes and type 2 diabetes
- Abdominal fat gain
- Chronic inflammation
- Cardiovascular disease
A deeper breakdown of symptoms, causes, and solutions is covered here:
👉 Understanding Insulin Resistance: Symptoms, Causes, and Solutions
https://thehealthknowledgebase.com/blood-sugar/what-is-insulin-resistance/
Long-Term Risks of Poor Glucose Control
Unmanaged blood sugar affects far more than energy levels. Long-term dysregulation is linked to:
- Heart disease and stroke
- Cognitive decline and dementia
- Nerve damage and poor circulation
- Hormonal imbalances
- Accelerated aging
The good news: insulin sensitivity can be improved at nearly any age with the right strategies.
3. Knowing Your Numbers: Measurement Matters
You cannot manage what you do not measure.
Common Blood Sugar Testing Methods
Fasting Blood Glucose
Measures baseline glucose after an overnight fast.
HbA1c
Shows your average blood sugar over the past 2–3 months.
Continuous Glucose Monitors (CGMs)
Track glucose levels in real time and reveal how food, sleep, stress, and exercise affect you personally.
A complete non-diabetic CGM guide is available here:
👉 How to Use a Continuous Glucose Monitor (CGM) for Metabolic Health
https://thehealthknowledgebase.com/blood-sugar/cgm-guide-non-diabetics/
Understanding Blood Sugar Ranges
Knowing what is normal — and what is not — is critical.
For a detailed chart by age and condition, see:
👉 Normal Blood Sugar Levels Chart: A Guide for Every Age Group
https://thehealthknowledgebase.com/blood-sugar/blood-sugar-levels-chart/
As a general reference:
- Optimal fasting glucose is typically below 90 mg/dL
- Persistent readings above 100 mg/dL may indicate insulin resistance
4. The Pillars of Natural Blood Sugar Management
Pillar 1: Nutrition and “The Plate”
Food composition matters more than calories alone.
The most effective blood sugar–friendly plate includes:
- High fiber (vegetables, legumes, seeds)
- Adequate protein (fish, eggs, poultry, tofu)
- Healthy fats (olive oil, avocado, nuts)
Carbohydrates are not eliminated — they are strategically managed.
Understanding glycemic load and food quality is essential. Start here:
👉 15 Low-Glycemic Foods That Won’t Spike Your Insulin
https://thehealthknowledgebase.com/blood-sugar/best-low-gi-foods/
Pillar 2: Movement and Muscle
Muscle tissue is a powerful glucose sink.
Even light activity improves glucose uptake — and timing matters.
One of the most effective strategies is simple walking after meals:
👉 Post-Meal Walking: The 10-Minute Secret to Glucose Control
https://thehealthknowledgebase.com/blood-sugar/walking-after-meals-benefits/
Resistance training also increases insulin sensitivity by expanding muscle mass, allowing glucose to be stored efficiently instead of circulating in the blood.
Pillar 3: Stress and Sleep Regulation
Stress hormones directly raise blood sugar by signaling the liver to release glucose.
Chronic cortisol elevation makes insulin resistance worse, even with a perfect diet.
Learn how stress affects glucose — and how to counteract it:
👉 How Stress Spikes Your Blood Sugar (and 3 Remedies to Stop It)
https://thehealthknowledgebase.com/blood-sugar/stress-and-glucose-levels/
Sleep deprivation further compounds the problem by impairing insulin signaling:
👉 The Relationship Between Sleep Deprivation and Insulin Resistance
https://thehealthknowledgebase.com/blood-sugar/sleep-and-blood-sugar/
5. Smart Supplementation: Science-Backed Support
This section serves as a navigation hub for your supplement cluster.
Evidence-Supported Ingredients
- Berberine — improves insulin sensitivity similarly to some medications
👉 https://thehealthknowledgebase.com/blood-sugar/berberine-vs-metformin/ - Cinnamon — may modestly reduce fasting glucose
👉 https://thehealthknowledgebase.com/blood-sugar/cinnamon-for-blood-sugar/ - Alpha-Lipoic Acid (ALA) — supports nerve health and glucose metabolism
👉 https://thehealthknowledgebase.com/blood-sugar/alpha-lipoic-acid-benefits/ - Magnesium — critical for insulin signaling
👉 https://thehealthknowledgebase.com/blood-sugar/magnesium-for-blood-sugar/
Supplement comparisons and rankings are covered here:
👉 10 Best Blood Sugar Supplements of 2025
https://thehealthknowledgebase.com/blood-sugar/best-supplements-review/
Always consult a healthcare professional if using medication.
6. Lifestyle “Hacks” for Immediate Impact
Eat in the Right Order
Fiber → Protein/Fats → Carbohydrates
This sequence slows glucose absorption.
Apple Cider Vinegar
Vinegar before meals may blunt post-meal glucose spikes:
👉 https://thehealthknowledgebase.com/blood-sugar/apple-cider-vinegar-glucose-hack/
Hydration
Adequate water intake helps the kidneys clear excess glucose and supports metabolic efficiency.
7. Troubleshooting Common Challenges
Dawn Phenomenon
Morning glucose spikes caused by overnight hormone release.
Reactive Hypoglycemia
Post-meal crashes triggered by rapid insulin release.
Hidden Sugars
Many “healthy” foods contain unexpected glucose triggers:
👉 https://thehealthknowledgebase.com/blood-sugar/hidden-sugars-in-foods/
8. Conclusion: Building a Sustainable Blood Sugar Strategy
Blood sugar management is not about perfection — it is about consistency.
Small, repeatable wins compound:
- Balanced meals
- Daily movement
- Quality sleep
- Stress regulation
When these habits align, insulin sensitivity improves naturally, energy stabilizes, and long-term health outcomes follow.
This guide is your foundation. The supporting articles in this silo will help you personalize and refine your approach over time.
FAQs
- What is the fastest natural way to lower blood sugar?
A brisk 10–20 minute walk after a meal, hydration, and reducing high-glycemic carbs are among the fastest lifestyle actions. For a deeper “quick response” guide, see: https://thehealthknowledgebase.com/blood-sugar/how-to-lower-blood-sugar-quickly/ - What causes blood sugar spikes even when eating “healthy” foods?
Hidden sugars, refined starches, low fiber meals, stress, poor sleep, and eating carbs alone can all trigger spikes. Many packaged “health foods” still contain glucose-spiking ingredients. See: https://thehealthknowledgebase.com/blood-sugar/hidden-sugars-in-foods/ - Can non-diabetics benefit from tracking glucose?
Yes. A CGM can reveal personal trigger foods, stress effects, sleep impact, and meal timing patterns—helpful for metabolic health. See: https://thehealthknowledgebase.com/blood-sugar/cgm-guide-non-diabetics/ - What is insulin resistance in simple terms?
It means your cells stop responding efficiently to insulin, so the body needs more insulin to move glucose into cells. Over time, this can lead to prediabetes and type 2 diabetes. See: https://thehealthknowledgebase.com/blood-sugar/what-is-insulin-resistance/ - Do low-glycemic foods really help?
They often help because they digest more slowly and reduce post-meal spikes—especially when combined with protein, fiber, and healthy fats. See: https://thehealthknowledgebase.com/blood-sugar/best-low-gi-foods/ - What’s the best exercise for blood sugar control?
Walking after meals is one of the most consistent “high ROI” habits, and resistance training improves insulin sensitivity long-term. Start here: https://thehealthknowledgebase.com/blood-sugar/walking-after-meals-benefits/ - How does stress raise blood sugar?
Stress hormones (especially cortisol and adrenaline) signal the liver to release glucose into the blood—useful in emergencies, harmful when chronic. See: https://thehealthknowledgebase.com/blood-sugar/stress-and-glucose-levels/ - Does sleep affect insulin sensitivity?
Yes. Poor sleep reduces insulin sensitivity and increases cravings and hunger hormones, making glucose control harder the next day. See: https://thehealthknowledgebase.com/blood-sugar/sleep-and-blood-sugar/ - Which supplements have the best evidence for glucose control?
Berberine, magnesium (when deficient), ALA (especially for nerve support), and cinnamon show varying levels of evidence depending on the person. Start with the reviews hub: https://thehealthknowledgebase.com/blood-sugar/best-supplements-review/ - What is the “dawn phenomenon” and should I worry?
It’s a morning glucose rise driven by hormones that increase blood sugar to help you wake up. It can be more pronounced with insulin resistance. If persistent or extreme, it’s worth discussing with a clinician and addressing sleep, dinner composition, and activity patterns.
Want a step-by-step plan to stabilize your blood sugar naturally?
Explore the Blood Sugar Hub for CGM guidance, glucose spike strategies, low-GI foods, stress & sleep fixes, and science-backed supplement breakdowns.