You’ve tried the inhalers. You’ve taken the allergy meds. You’ve swallowed countless cough syrups. Yet, that persistent tickle in your throat, the unexplained wheeze, and the feeling of a constant lump won’t go away.
What if the problem isn’t in your lungs at all, but is silently rising from your gut?
This is the reality of Laryngopharyngeal Reflux (LPR), often called “silent reflux.” Unlike its cousin GERD, which announces itself with fiery heartburn, LPR operates in the shadows. It’s a stealthy condition where stomach contents creep up and silently damage your throat, sinuses, and—most critically—your airways. Understanding this gut-lung axis is the key to unlocking a mystery that plagues millions.
What is Silent Reflux (LPR)? The Stealth Bomber of Digestive Issues
If classic acid reflux (GERD) is a volcano, silent reflux (LPR) is its toxic, invisible gas cloud.
While GERD involves acidic liquid reflux that burns the esophagus, LPR is characterized by the rise of acidic gas, mist, or aerosols. This mist contains not just acid, but also a potent digestive enzyme called pepsin.
The critical difference? This mist travels much higher. It bypasses the esophagus and passes through the upper esophageal sphincter, reaching your highly sensitive throat (larynx), vocal cords, and even the openings to your lungs and sinuses. The tissues there have no protection against stomach juices, leading to inflammation and damage without the classic sign of heartburn.
5 Silent Signs Reflux is Choking Your Airways (Not Allergies)
If you identify with several of these, your breathing issues may have a hidden, digestive root cause.
1. The Mystery Morning Hoarseness & Constant Throat Clearing
Your vocal cords are extremely delicate. When pepsin and acid land on them, they become inflamed and swollen, leading to a deeper, raspier voice—especially upon waking. The irritation also creates a persistent feeling that something is stuck, triggering a compulsive need to clear your throat, a topic we explore in depth in Why Am I Always Clearing My Throat? (Not Allergies).
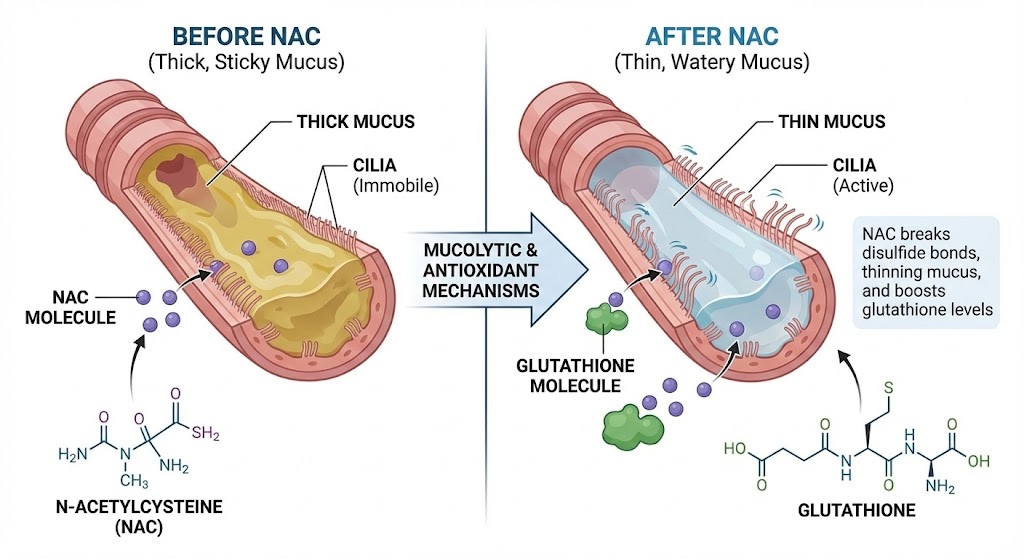
2. The Mucus Trap: The Feeling of a Permanent “Lump” (Globus Sensation)
This isn’t imagination. Your throat is producing extra thick mucus as a defense mechanism to shield itself from the corrosive reflux. This creates the classic “globus sensation”—a feeling of a lump or ball in your throat that doesn’t go away with swallowing.
3. The Asthmatic Wheeze (Especially After Meals or Lying Down)
When the reflux mist is inhaled into the airways (microaspiration), it irritates the bronchial tubes, causing them to swell and spasm. This results in wheezing, chest tightness, and shortness of breath that is often mistaken for asthma. If your symptoms flare up after a large meal or when you lie down at night, reflux is a prime suspect.
4. The Unshakeable “Post-Nasal Drip” & Chronic Cough
The reflux mist can irritate the back of your nasal passages and sinuses, tricking them into producing excess mucus. This drains down the back of your throat, feeling like post-nasal drip and triggering a relentless, dry cough. This nighttime coughing is a classic sign, as lying flat makes reflux easier.
5. Waking Up Gasping or with Shortness of Breath
In severe cases, the irritation can cause a sudden, reflexive spasm of the vocal cords (laryngospasm). This closes off your airway momentarily, causing you to wake up gasping for air in a panic. It’s a terrifying experience and a major red flag for significant LPR.
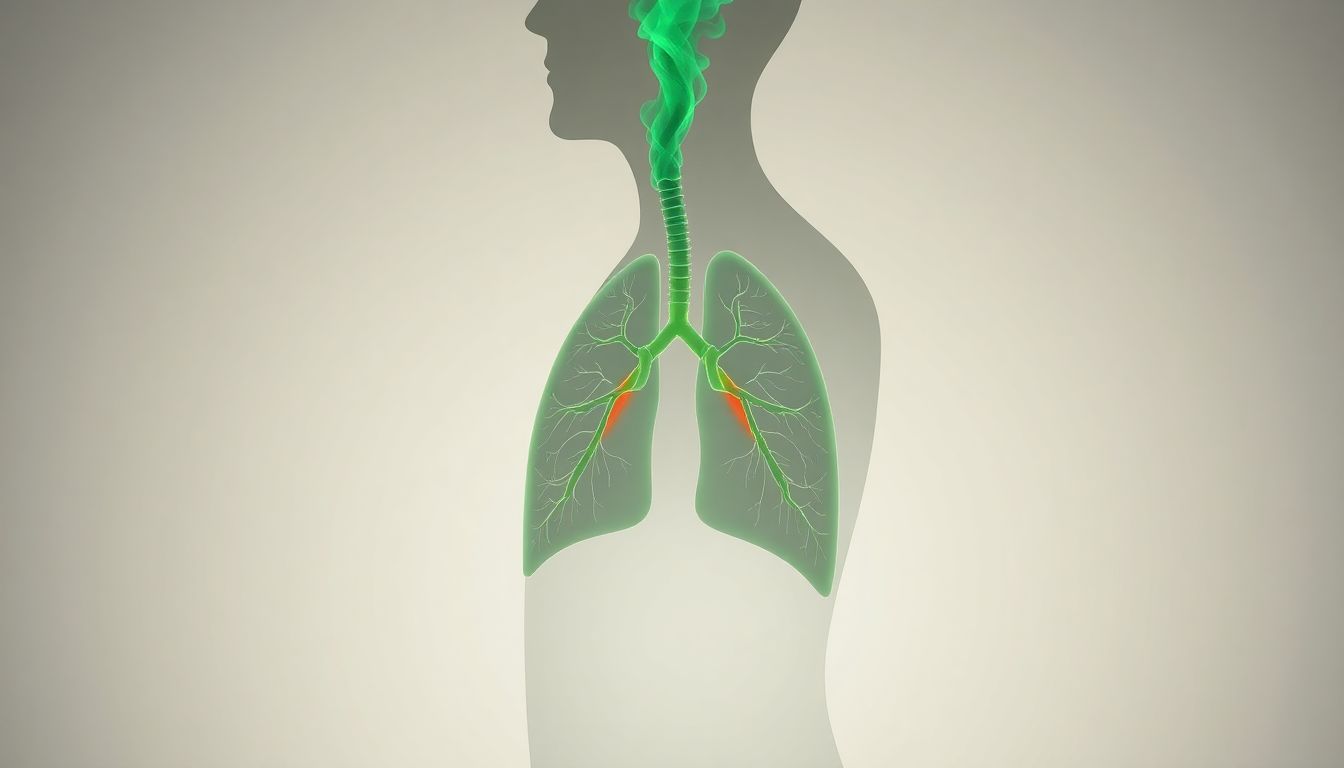
The Vicious Cycle: How Reflux Secretly Damages Your Lungs
The reflux-lung connection creates a self-perpetuating nightmare:
- Reflux Event: Stomach mist containing acid and pepsin travels up.
- Airway Irritation: The mist inflames your throat, vocal cords, and bronchial tubes.
- Breathing Difficulty: Inflammation causes swelling, mucus production, and bronchospasm, leading to coughing and shortness of breath.
- Increased Pressure: Coughing and labored breathing increase pressure in your abdomen.
- Worsened Reflux: This abdominal pressure forces more stomach contents upward, restarting the cycle.
This cycle is often mediated by the vagus nerve, which plays a key role in both digestion and respiratory reflexes.
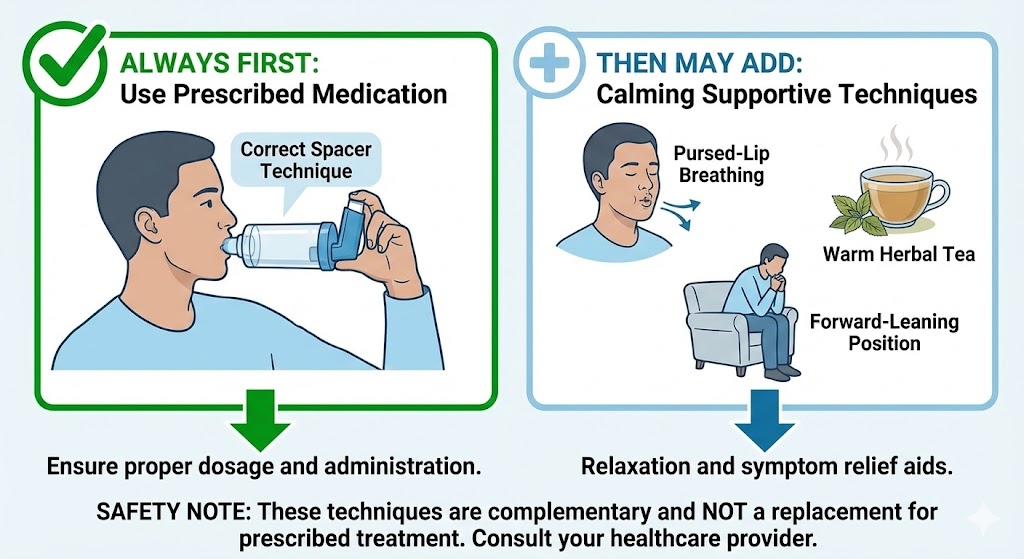
The 3-Step Protocol to Break the Reflux-Lung Cycle
Breaking this cycle requires a consistent, multi-pronged approach. Medication alone often isn’t enough.
Step 1: The Reflux-Smart Diet & Eating Habits
This is the most critical step. You must starve the reflux.
- Eliminate Top Triggers: The biggest offenders are coffee, alcohol, chocolate, spicy foods, fried/fatty foods, tomatoes, and citrus.
- Embrace Alkaline Foods: Incorporate bananas, melons, oatmeal, green vegetables, and almonds.
- Adopt Key Habits:
- Eat Smaller Meals: Large meals distend the stomach and increase pressure.
- Finish Eating 3-4 Hours Before Bed: Give your stomach time to empty before you lie down.
- Eat Upright and Chew Thoroughly: Don’t eat on the go or while slouching.
Step 2: The Gravity-Guard Nighttime Routine
Use gravity as your ally while you sleep.
- Elevate the Head of Your Bed: Place 4-6 inch blocks under the bedposts at the head of your bed. Do not just stack pillows, as this can kink your abdomen and make reflux worse.
- Sleep on Your Left Side: Anatomy makes reflux less likely in this position.
- Wear Loose-Fitting Clothing: Avoid any tightness around your waist, especially at night.
Step 3: Targeted Natural Remedies to Soothe & Heal
- Alkaline Water: Sipping alkaline water (pH > 8.5) between meals can help neutralize acid and deactivate pepsin in the throat.
- D-Limonene: A supplement derived from orange peel that can help clear stagnant stomach contents and improve LES function.
- Deglycyrrhizinated Licorice (DGL): This form of licorice soothes and protects the mucosal lining of the esophagus and throat without affecting blood pressure.
- Alginate Formulas (e.g., Gaviscon Advance): These create a protective “raft” on top of your stomach contents, acting as a physical barrier against reflux.
Integrating these steps with foundational breathing practices, like those in our guide to diaphragmatic breathing, can further help by optimizing pressure dynamics in your core.
When to See a Doctor: Red Flags & Diagnostic Tests
If your symptoms are severe or don’t improve with lifestyle changes, see an ENT or Gastroenterologist.
- Red Flags: Difficulty swallowing, persistent pain, unintended weight loss, or choking episodes.
- Diagnostic Tests: They may recommend a Laryngoscopy (to see vocal cord damage), 24-hour pH-Impedance Study (the gold standard for detecting non-acid reflux), or Esophageal Manometry (to measure muscle function).
Conclusion: You Can Breathe Freely Again
The journey to solving chronic cough and breathing problems often requires playing medical detective. By understanding the silent reflux-lung connection, you’ve uncovered a potential root cause that countless others—and even some doctors—overlook.
This isn’t a life sentence. By implementing this 3-step protocol consistently, you can quiet the reflux, calm the inflammation, and break the vicious cycle for good. Your path to peaceful nights and clear, easy breathing starts today.
FAQs
1. Can silent reflux cause permanent lung damage?
Yes, chronic, untreated silent reflux can lead to conditions like chronic bronchitis, bronchiectasis, and can worsen asthma, causing permanent changes to the airways over time.
2. How is silent reflux (LPR) different from GERD?
GERD primarily causes heartburn and regurgitation due to liquid acid in the esophagus. LPR, or “silent reflux,” causes symptoms higher up—like hoarseness, throat clearing, and cough—due to a gas/mist that reaches the throat and lungs, often without heartburn.
3. What is the fastest way to relieve silent reflux symptoms?
Immediate relief can come from sipping alkaline water to deactivate pepsin. For long-term relief, the most impactful step is to stop eating at least 3 hours before bedtime and strictly avoid dietary triggers like coffee and alcohol.
4. Can silent reflux feel like an asthma attack?
Absolutely. When reflux is inhaled into the airways, it can cause bronchospasm—a sudden constriction of the airway muscles—leading to wheezing, chest tightness, and shortness of breath that is indistinguishable from an asthma attack.
5. What is the best sleeping position for silent reflux?
Sleeping on your left side is best, as anatomy makes it harder for reflux to occur. Most importantly, elevate the head of your entire bed by 4-6 inches to use gravity as a barrier.
6. Can stress cause silent reflux?
Yes, stress is a major contributor. It can increase stomach acid production, delay stomach emptying, and make you more sensitive to the effects of reflux, creating a vicious cycle explored in our article on the lung-brain feedback loop.
7. Are there any long-term solutions for LPR?
While some may need long-term dietary management, many people can resolve their LPR by consistently following a reflux-smart diet, optimizing their sleep position, achieving a healthy weight, and managing stress, which allows the throat and airway tissues to heal.
8. Can silent reflux cause excessive mucus and post-nasal drip?
Yes, this is one of the most common symptoms. The throat and sinuses produce extra thick mucus as a protective mechanism against the irritating reflux mist, leading to a constant feeling of post-nasal drip and the need to clear your throat.
9. Is silent reflux common after quitting smoking?
It can be. While quitting is crucial for healing your lungs, some people experience a temporary increase in reflux symptoms due to changes in digestion and the absence of nicotine, which can have a mild suppressing effect on stomach acid.
10. What kind of doctor should I see for silent reflux?
Start with an Ear, Nose, and Throat (ENT) doctor, as they can perform a laryngoscopy to see the physical signs of reflux on your vocal cords. A Gastroenterologist (GI) is also an excellent choice for more comprehensive testing like a pH study.
Still Have Questions? We Have Answers.
Lung health is complex. If you’re wondering “What about…?” or “What’s next for me?”, you’re not alone. Our Resource Hub is built to be your **first stop for trustworthy, in-depth answers** on every aspect of respiratory wellness.
- Condition-Specific Guides (COPD, Asthma, Post-COVID)
- Step-by-Step Detox & Recovery Plans
- Science-Backed Natural & Conventional Strategies