That sudden feeling of not being able to get enough air – it’s one of the most frightening sensations our bodies can produce. But what if you could decode what your breathlessness is trying to tell you?
Not all shortness of breath is created equal. The pattern, timing, and accompanying symptoms of your breathing difficulties reveal crucial information about whether the issue originates in your heart, lungs, or nervous system. Understanding these differences isn’t just academic – it can guide you toward the right solutions and help you know when to seek urgent care.
Type 1: Cardiac Shortness of Breath – When Your Heart Can’t Keep Up
What it feels like: “I can’t breathe when I lie down flat” or “I wake up gasping for air”
Cardiac-related breathlessness occurs when your heart struggles to pump blood efficiently, causing fluid to back up into your lungs. This is medically known as pulmonary edema.
Key Identifiers:
- Worse when lying flat (orthopnea) – often requires 2-3 pillows to sleep
- Paroxysmal nocturnal dyspnea – waking up 1-2 hours after falling asleep, gasping for air
- Improves when sitting up or standing
- Associated with swelling in ankles, legs, or abdomen
- Often accompanied by fatigue, reduced exercise tolerance, and sometimes chest pain
Common Causes: Heart failure, coronary artery disease, arrhythmias, valve problems
What to Do: If you experience breathing difficulties that improve when sitting up, especially with leg swelling, this warrants prompt medical evaluation. This type of breathlessness can signal serious cardiac issues that need attention.
Type 2: Respiratory Shortness of Breath – When Your Lungs Struggle
What it feels like: “I can’t get air out” or “There’s a tight band around my chest”
Respiratory breathlessness stems from problems in your lungs or airways themselves, making it difficult to move air in or out effectively.
Key Identifiers:
- Wheezing or whistling sounds when breathing
- Persistent cough, often with mucus production
- Feeling of incomplete exhalation
- Triggered by allergens, exercise, or respiratory infections
- Relieved by specific positions or breathing techniques
Common Causes: Asthma, COPD, pulmonary fibrosis, pneumonia, Post-COVID Lung Recovery
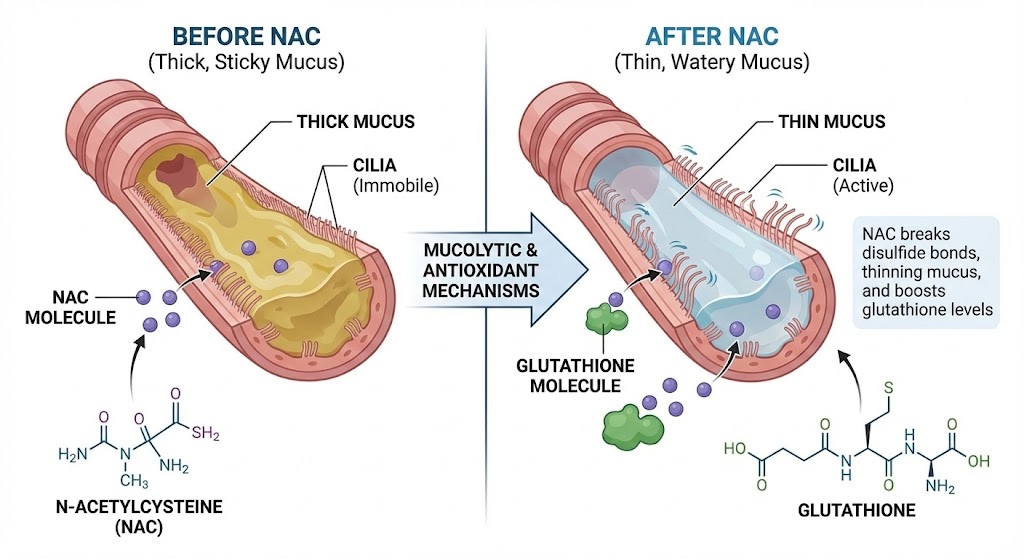
The Mucus Connection: Many respiratory causes involve mucus buildup that obstructs airways. If you’re dealing with persistent congestion, our Mucus Color Chart: What Your Phlegm Says can help you understand what’s happening.
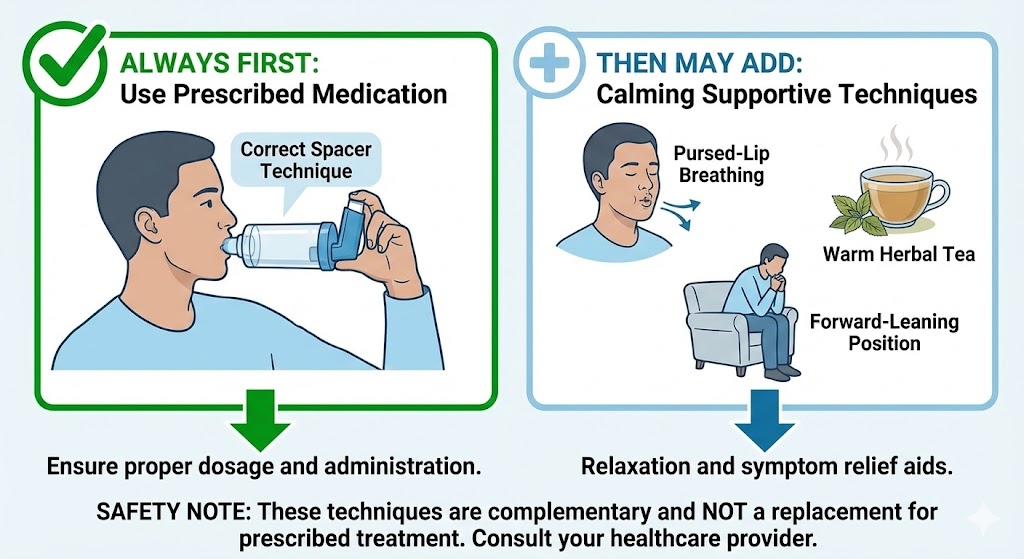
Breathing Techniques That Help: For respiratory breathlessness, specific techniques can provide immediate relief. Learn Pursed-Lip Breathing: How to Stop Shortness of Breath Instantly and Diaphragmatic Breathing: The #1 Exercise to Strengthen Your Lungs.
Type 3: Anxiety-Related Shortness of Breath – When Your Brain Sends False Alarms
What it feels like: “I can’t get a deep enough breath” or “I’m breathing but not getting enough oxygen”
This type stems from your nervous system, where anxiety or panic triggers rapid, shallow breathing that actually reduces oxygen delivery to your tissues.
Key Identifiers:
- Sudden onset during stressful situations
- Hyperventilation – breathing too fast and too shallow
- Tingling in fingers, lips, or face
- Feeling of detachment or unreality
- No positional relief – doesn’t improve with sitting or standing
- Often accompanied by racing thoughts, pounding heart, sweating
Common Causes: Panic disorder, generalized anxiety, stress-induced hyperventilation
The Vagus Nerve Connection: Your vagus nerve plays a crucial role in anxiety-related breathing. When it’s dysregulated, it can trigger false alarm signals. Learn how to calm this system in The Vagus Nerve & Your Lungs: The Missing Link to Calming Coughs.
Quick Identification Guide
| Symptom | Cardiac | Respiratory | Anxiety |
|---|---|---|---|
| Position affects it | ✓ Improves sitting up | Sometimes | ✗ No effect |
| Cough | Sometimes dry cough | ✓ Often with mucus | ✗ Rare |
| Wheezing | ✗ No | ✓ Common | ✗ No |
| Onset | Gradual worsening | Variable | ✓ Sudden |
| Swelling | ✓ Common | ✗ Rare | ✗ No |
| Tingling | ✗ No | ✗ No | ✓ Common |
When to Seek Immediate Medical Attention
Certain symptoms with shortness of breath require urgent evaluation:
- Chest pain or pressure
- Blue-tinged lips or fingernails
- Confusion or difficulty speaking
- Rapid heart rate that doesn’t slow with rest
- Fainting or near-fainting
- Severe lightheadedness
If you’re unsure about your symptoms, our guide Is It Asthma or Something Else? 5 Conditions Often Misdiagnosed can provide additional clarity.
Natural Management Strategies Based on Your Type
For Cardiac Patterns:
- Elevate your head during sleep
- Monitor fluid intake if recommended by your doctor
- Practice gentle movement like walking
- Manage stress through meditation
For Respiratory Patterns:
- Practice breathing exercises daily
- Use The Power of Steam: How to Use Inhalation for Instant Mucus Relief
- Consider natural expectorants like Mullein for Lungs: The Ancient Herb That Melts Mucus
- Avoid environmental triggers when possible
For Anxiety Patterns:
- Practice grounding techniques during episodes
- Learn vagus nerve stimulation exercises
- Use the 4-7-8 breathing technique (inhale 4, hold 7, exhale 8)
- Consider professional support for anxiety management
The Bottom Line: Knowledge is Power
Understanding the differences between cardiac, respiratory, and anxiety-related shortness of breath empowers you to take appropriate action. While this guide helps you identify patterns, remember that any persistent breathing difficulties warrant professional medical evaluation.
Your breathing patterns are messengers—learning to understand their language is the first step toward addressing the root causes and finding lasting relief.
Still Have Questions? We Have Answers.
Lung health is complex. If you’re wondering “What about…?” or “What’s next for me?”, you’re not alone. Our Resource Hub is built to be your **first stop for trustworthy, in-depth answers** on every aspect of respiratory wellness.
- Condition-Specific Guides (COPD, Asthma, Post-COVID)
- Step-by-Step Detox & Recovery Plans
- Science-Backed Natural & Conventional Strategies