The lingering breathlessness, the persistent cough, the crushing fatigue – if you’re among the millions struggling with respiratory symptoms long after your COVID infection has passed, you know the frustration of feeling like your lungs have forgotten how to breathe.
Post-COVID lung damage isn’t just in your head, and it’s not something you have to “just live with.” Emerging research shows that with the right approach, lung tissue can heal and function can be restored. This 90-day plan combines the latest medical understanding with proven natural strategies to help you reclaim your breathing and your life.
Understanding Post-COVID Lung Damage: What Actually Happened to Your Lungs
COVID-19 can affect the respiratory system in several distinct ways, and understanding your specific type of damage is the first step toward targeted recovery:
1. Airway Inflammation and Sensitivity
The virus triggers an intense inflammatory response that can leave your airways hypersensitive and reactive, similar to asthma. This explains why many people develop new-onset wheezing or coughing fits after COVID.
2. Alveolar Damage
The tiny air sacs (alveoli) where oxygen exchange occurs can become damaged or scarred, reducing your lungs’ efficiency. This is often reflected in lower oxygen saturation levels, especially during activity.
3. Diaphragm and Respiratory Muscle Weakness
Prolonged illness and inflammation can weaken the muscles responsible for breathing, making each breath require more effort. This is why you might feel breathless even during simple tasks.
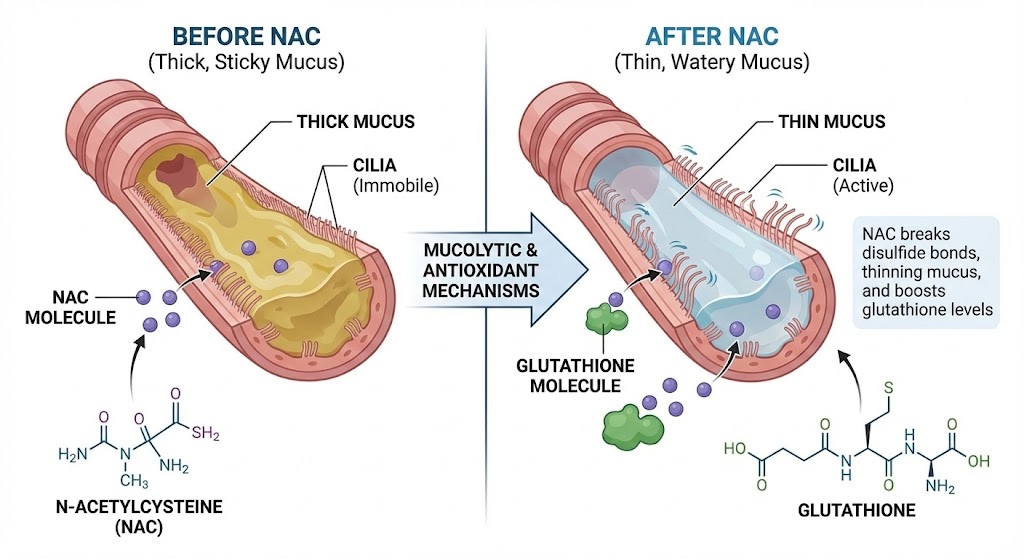
4. Mucus Production Changes
Many post-COVID patients report thicker, stickier mucus that’s harder to clear, leading to that constant feeling of congestion and the need to repeatedly clear your throat.
If you’re experiencing persistent throat clearing, our guide Why Am I Always Clearing My Throat? (Not Allergies) can help you understand the mechanisms behind this frustrating symptom.
The 90-Day Post-COVID Lung Recovery Plan
This phased approach recognizes that healing takes time and that pushing too hard too soon can set back your progress.
Days 1-30: The Foundation Phase – Calming Inflammation & Rebuilding Basics
Week 1-2: Gentle Reactivation
- Breathing Focus: Practice Diaphragmatic Breathing: The #1 Exercise to Strengthen Your Lungs & Calm Your Mind for 5 minutes, 2x daily
- Movement: 5-10 minute slow walks daily, focusing on nasal breathing
- Nutrition: Anti-inflammatory foods from The Lungs’ Best Friends: Top 5 Anti-Inflammatory Foods for Breathing
- Monitoring: Track your oxygen saturation before and after activity
Week 3-4: Building Consistency
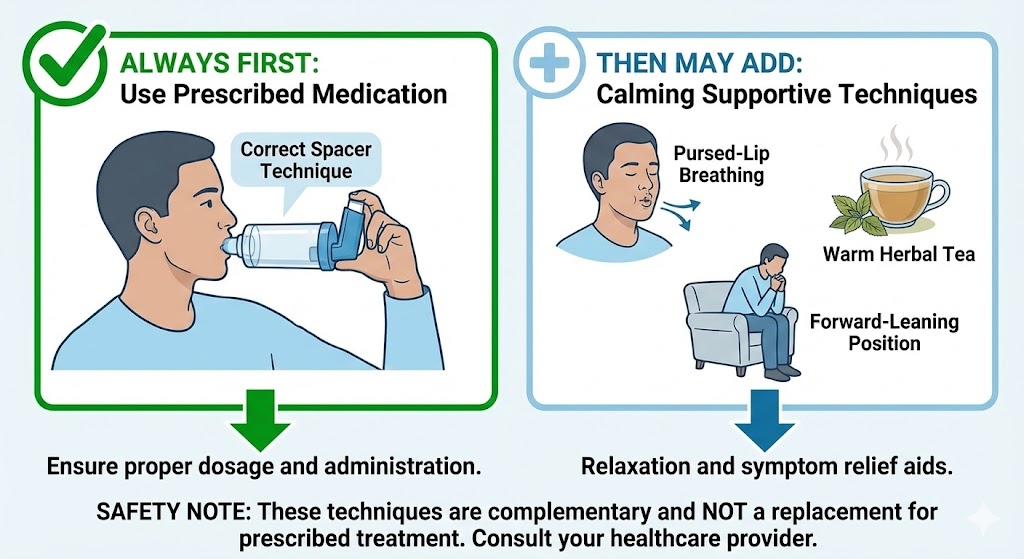
- Breathing Focus: Add Pursed-Lip Breathing: How to Stop Shortness of Breath Instantly during walks
- Movement: Increase to 15-minute walks, incorporating gentle hills if tolerated
- Mucus Management: Begin steam inhalation using techniques from The Power of Steam: How to Use Inhalation for Instant Mucus Relief
Days 31-60: The Rebuilding Phase – Increasing Capacity & Strength
Week 5-8: Progressive Training
- Breathing Focus: Introduce interval breathing – 30 seconds deep breaths, 30 seconds normal breathing
- Movement: 20-30 minute walks with brief periods of faster pacing
- Strength: Begin Best Yoga Poses for Lung Capacity and Chest Opening 3x weekly
- Support: Consider natural anti-inflammatories from Herbs and Spices for Respiratory Health: Beyond Mullein
Days 61-90: The Optimization Phase – Restoring Full Function
Week 9-12: Integration & Maintenance
- Breathing Focus: Practice speaking while walking to build respiratory endurance
- Movement: Return to 75% of your pre-COVID activity level
- Maintenance: Establish your The 10-Minute Daily Lung Maintenance Routine
- Long-term Health: Continue with lung-supporting nutrition and breathing exercises
Essential Tools for Your Recovery Journey
1. Pulse Oximeter: Your Progress Tracker
Don’t guess about your oxygen levels. A simple finger pulse oximeter provides objective data about your improvement. Look for:
- Consistent readings above 95% at rest
- Less than 4% drop in saturation during activity
- Faster recovery to baseline after exertion
2. Breathing Pacemaker: The Vagus Nerve Connection
Your vagus nerve plays a crucial role in respiratory recovery after viral illness. Techniques that stimulate this nerve can reduce inflammation and improve breathing efficiency. Learn specific methods in The Vagus Nerve & Your Lungs: The Missing Link to Calming Coughs.
3. Mucus Management Strategies
For stubborn post-COVID congestion, you may need more targeted approaches:
- Positioning: Use techniques from Postural Drainage: Simple Positions to Drain Mucus from Your Lungs
- Supplement Support: Consider NAC (N-Acetylcysteine): How This Hospital-Grade Supplement Breaks Down Stubborn Mucus
Nutritional Support for Lung Tissue Repair
Your diet provides the building blocks for healing. Focus on these key elements:
Protein-Rich Foods: Essential for tissue repair (eggs, fish, legumes, lean meats)
Vitamin C: Supports collagen production for lung structure (citrus, bell peppers, broccoli)
Omega-3 Fatty Acids: Reduce inflammation (fatty fish, walnuts, flaxseeds)
Antioxidant-Rich Foods: Protect against oxidative damage (berries, dark leafy greens, green tea)
For delicious, lung-supporting recipes, try The Ultimate Lung-Health Smoothie: 3 Recipes to Reduce Mucus & Fight Inflammation.
When to Seek Specialized Help
While this plan helps most people with post-COVID breathing issues, consult your healthcare provider if you experience:
- Oxygen saturation consistently below 92%
- Chest pain or palpitations
- Dizziness or confusion
- Symptoms that worsen despite following recovery protocols
If you’re unsure whether your symptoms are COVID-related or something else, our guide Is It Asthma or Something Else? 5 Conditions Often Misdiagnosed can provide clarity.
Success Stories: Real People, Real Recovery
“After 8 months of struggling with post-COVID breathing issues, I started the 90-day plan. By day 45, I could walk up my driveway without stopping to catch my breath. By day 90, I was back to hiking gentle trails. The phased approach kept me from pushing too hard and getting discouraged.” – Mark, 52
“The combination of breathing exercises and the nutritional advice made all the difference. I learned that I wasn’t ‘broken’ forever—my lungs just needed the right kind of rehabilitation.” – Sarah, 38
The Bottom Line: Your Lungs Can Heal
Post-COVID lung recovery is a journey, not a destination. Some days will be better than others, and that’s normal. The key is consistency and listening to your body while gently challenging your limits.
Remember that healing occurs in phases, and the 90-day framework provides structure while allowing flexibility for your individual pace. Your lungs have remarkable regenerative capacity—they just need the right conditions and strategies to activate their innate healing intelligence.