You’ve taken the test. You blew into that machine as hard and as fast as you could, and now you’re holding a printout filled with graphs, numbers, and confusing acronyms like FEV1 and FVC. It might as well be in a foreign language.
Don’t let that piece of paper intimidate you. Understanding your spirometry results is a powerful step toward taking control of your respiratory health.
This guide will translate that medical jargon into plain English. We’ll walk you through the key numbers and graphs, so you can understand what your lungs are telling you and have a more confident, informed conversation with your doctor. This is a key part of the proactive monitoring we advocate for in our Ultimate Guide to Clearing Mucus & Restoring Lung Health Naturally.
What is Spirometry, Really?
In simple terms, spirometry is a breathing fitness test.
It measures how much air your lungs can hold and how quickly you can move that air in and out. Think of it like a report card for your lungs, grading both their size (volume) and speed (flow).
It’s one of the most important tools for diagnosing and monitoring conditions like asthma, COPD, and pulmonary fibrosis, and is often a first step after discussing symptoms like the different types of shortness of breath.
The 3 Key Numbers You Need to Understand
While the report may have dozens of values, focus on these three first. They tell 90% of the story.
1. FVC (Forced Vital Capacity)
- Plain English: Your Lung’s Total Size. This is the total amount of air you can forcibly blow out after taking the biggest breath you can.
- What it Means: A lower-than-expected FVC can suggest that your lungs are restricted or can’t fully expand, perhaps due to scarring (fibrosis) or weakness in the chest muscles.
2. FEV1 (Forced Expiratory Volume in 1 Second)
- Plain English: Your Lung’s Power & Speed. This is the amount of air you can blast out in the very first second of blowing.
- What it Means: This measures how open your airways are. If your airways are narrowed or blocked (from inflammation in asthma or from destroyed walls in COPD), you won’t be able to push air out quickly. The FEV1 will be low.
3. The FEV1/FVC Ratio
- Plain English: The “Obstruction Detector.” This is simply the FEV1 divided by the FVC, expressed as a percentage.
- What it Means: This is the most important number for diagnosing obstructive lung diseases. It answers the question: “What percentage of your total lung air can you blow out in one second?”
- In healthy lungs: You can blow out most of your air quickly (ratio is high, usually >70-75% for adults).
- With obstruction: The blockage slows you down, so a smaller percentage of your air gets out in the first second (ratio is low).
How to Interpret Your Results: The Simple Breakdown
Doctors compare your results to “predicted values” based on your age, height, sex, and ethnicity. Your results will be shown as a percentage of this predicted value.
Here’s a simple table to understand the patterns:
| Condition | FVC (Size) | FEV1 (Power) | FEV1/FVC Ratio (Obstruction) |
|---|---|---|---|
| Normal Lungs | Normal | Normal | Normal |
| Obstructive (e.g., COPD, Asthma) | Normal or Low | Low | Low |
| Restrictive (e.g., Pulmonary Fibrosis) | Low | Low (because total size is low) | Normal or High |
In a nutshell:
- Low FEV1/FVC Ratio? Think Obstruction (blocked airways).
- Low FVC but Normal Ratio? Think Restriction (smaller/lung stiffness).
A Walk-Through of a Sample Spirometry Graph
The graph, called a flow-volume loop, can look complicated, but you only need to understand its basic shape.
- A Normal Loop: Looks like a tall, pointy mountain.
- An Obstructive Pattern (COPD/Asthma): The mountain has a “scooped” or sagging appearance on the way down. This “scoop” represents the slow, difficult emptying of air due to narrowed airways.
- A Restrictive Pattern: The mountain is shorter and narrower than expected, but often maintains a relatively pointy shape because the airways themselves are open.
What to Do With This Information
1. Don’t Self-Diagnose. This guide is for understanding, not for making a medical diagnosis. Many factors can influence results.
2. Prepare for Your Doctor’s Visit. Now you can go in with intelligent questions:
* “My FEV1 is 65% of predicted. What does that mean for my daily activities?”
* “The graph looks ‘scooped.’ Does that confirm obstructive lung disease?”
* “How can I improve my numbers over time?”
3. Use it as a Baseline. Spirometry is most powerful when tracked over time. It can show if your condition is stable, improving with treatments like the natural remedies for COPD we discuss, or worsening.
Beyond the Basics: Other Terms You Might See
- PEF (Peak Expiratory Flow): The absolute fastest speed you can blow out air. It’s useful for daily monitoring with a peak flow meter.
- FEF 25-75%: Measures the flow of air in the middle part of your exhale. It can be an early indicator of small airway disease.
Conclusion: You Hold the Key to Understanding
That spirometry report is no longer a mysterious document. You now know that FVC is about size, FEV1 is about power, and their ratio is the key to detecting blocked airways.
Armed with this knowledge, you are no longer a passive recipient of care. You are an informed, empowered partner in your lung health journey. Take this understanding, discuss it with your physician, and use it to take the next steps toward restoring your lung health.
FAQs
1. What is a normal FEV1 score?
There is no single “normal” number. Your expected (or “predicted”) FEV1 is based on your age, height, sex, and ethnicity. A result is considered normal if it is 80% or more of that predicted value. For example, if your predicted FEV1 is 4.0 liters, a result of 3.2 liters or higher (80% of 4.0) would typically be in the normal range.
2. Can I do a spirometry test at home?
Yes, but with a caveat. While you can purchase handheld spirometers for home use, they are best for tracking trends if you already have a diagnosis. The initial diagnostic test must be done in a clinic with a calibrated machine and a technician to ensure you are performing the maneuver correctly for accurate results.
3. What’s the difference between spirometry and a peak flow meter?
A peak flow meter only measures one thing: your Peak Expiratory Flow (PEF), which is the fastest speed you can blow. Spirometry is a more comprehensive test that measures volumes (like FVC) and flows at different points in your breath, providing a much more detailed picture of lung function. It’s a core part of advanced lung monitoring.
4. How can I improve my spirometry results?
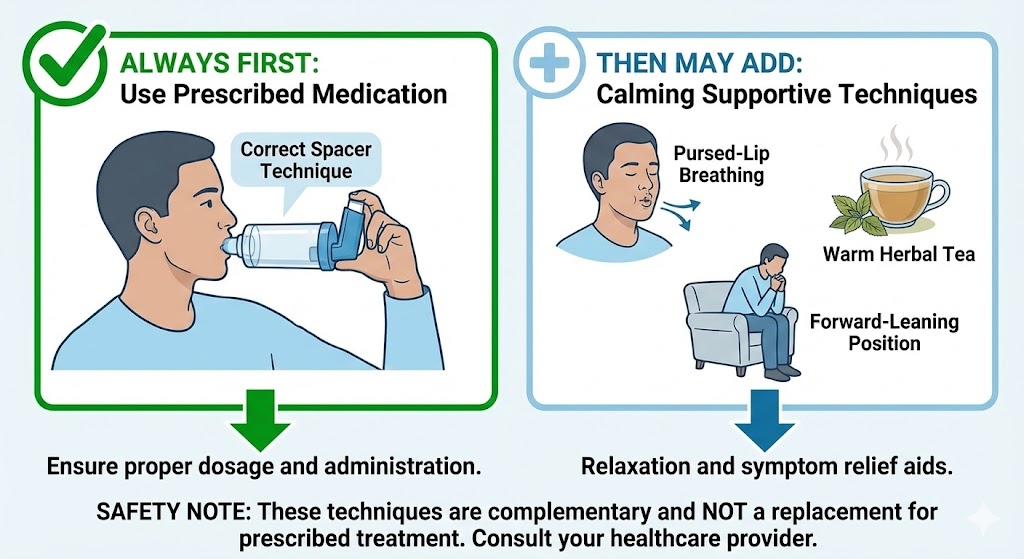
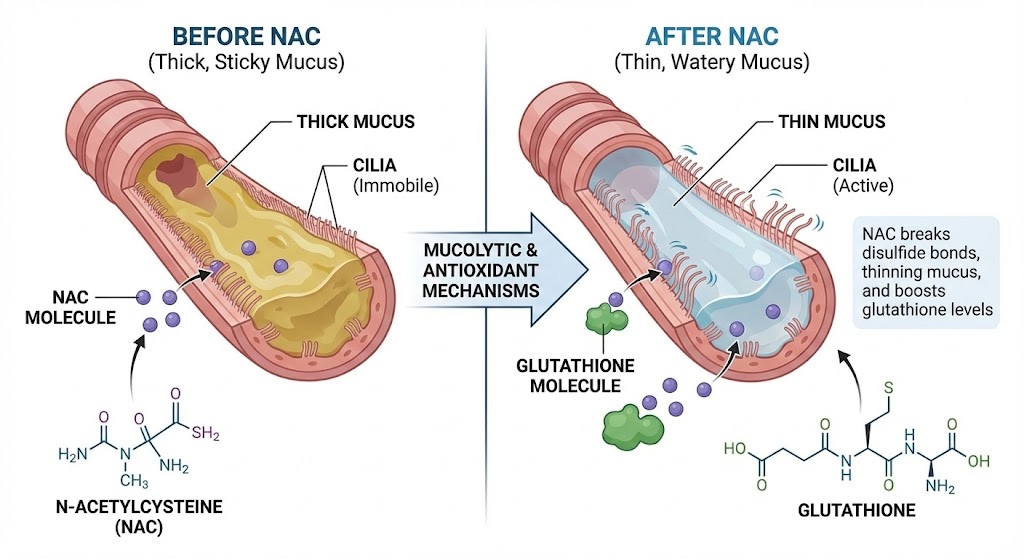
Improving your numbers depends on the underlying condition. For obstructive diseases like COPD and asthma, the key is reducing inflammation and opening airways through prescribed medications, breathing techniques like pursed-lip breathing, and avoiding irritants like smoke. Overall lung health can be supported by exercise and a healthy diet.
5. What does it mean if my FVC is low?
A low Forced Vital Capacity (FVC) suggests that your lungs are unable to fully expand. This is known as a “restrictive” pattern and can be caused by conditions that stiffen the lungs (like pulmonary fibrosis), affect the chest wall, or weaken the breathing muscles.
6. Can a spirometry test diagnose asthma?
Spirometry is a crucial tool for diagnosing asthma. A key indicator is that the FEV1 improves significantly (by more than 12%) after using a bronchodilator (quick-relief inhaler). This shows that the airway obstruction is reversible, which is a hallmark of asthma.
7. Why is the FEV1/FVC ratio so important?
The FEV1/FVC ratio is the primary indicator used to diagnose obstructive lung diseases like COPD and asthma. A low ratio means you have trouble moving air out of your lungs quickly, which is the definition of airway obstruction. It effectively separates obstructive diseases from restrictive ones.
8. What should I do before a spirometry test for accurate results?
For the most accurate results, you should: avoid smoking for at least 6-8 hours beforehand, avoid heavy meals, avoid alcohol, avoid strenuous exercise, and wear loose clothing. Also, inform your doctor about any medications you’re taking, as some may need to be withheld temporarily.
9. Can anxiety affect spirometry results?
Yes, anxiety can affect the test. If you are anxious, you may not be able to take a full, deep breath in or give a maximum, forceful blow out. It’s essential to try to relax and listen carefully to the technician’s instructions to ensure you’re performing the test correctly.
10. What is a bronchodilator reversibility test?
This is when the spirometry test is performed twice: first at baseline, and then again about 15 minutes after you’ve used a bronchodilator medication (like an albuterol inhaler). If your FEV1 improves significantly, it suggests your airways are responsive to medication, which is typical in asthma and can sometimes be seen in COPD.