The Unspoken Conversation: How BPH Affects Your Sexual Health
BPH is more than a bathroom issue – it’s a bedroom issue too. The physical changes in your prostate, the side effects of medications, and the stress of managing symptoms can all converge to impact your sexual health. Yet, this topic is often shrouded in silence, leaving men feeling isolated and uncertain.
If you’ve noticed changes in your erectile function, ejaculation, or libido since your BPH diagnosis, you’re not imagining things, and you’re certainly not alone. This guide breaks down the complex relationship between BPH and sexual health, offering clear explanations and practical strategies to help you maintain intimacy and satisfaction.
How BPH Directly and Indirectly Affects Sexual Function
The Physical Connection
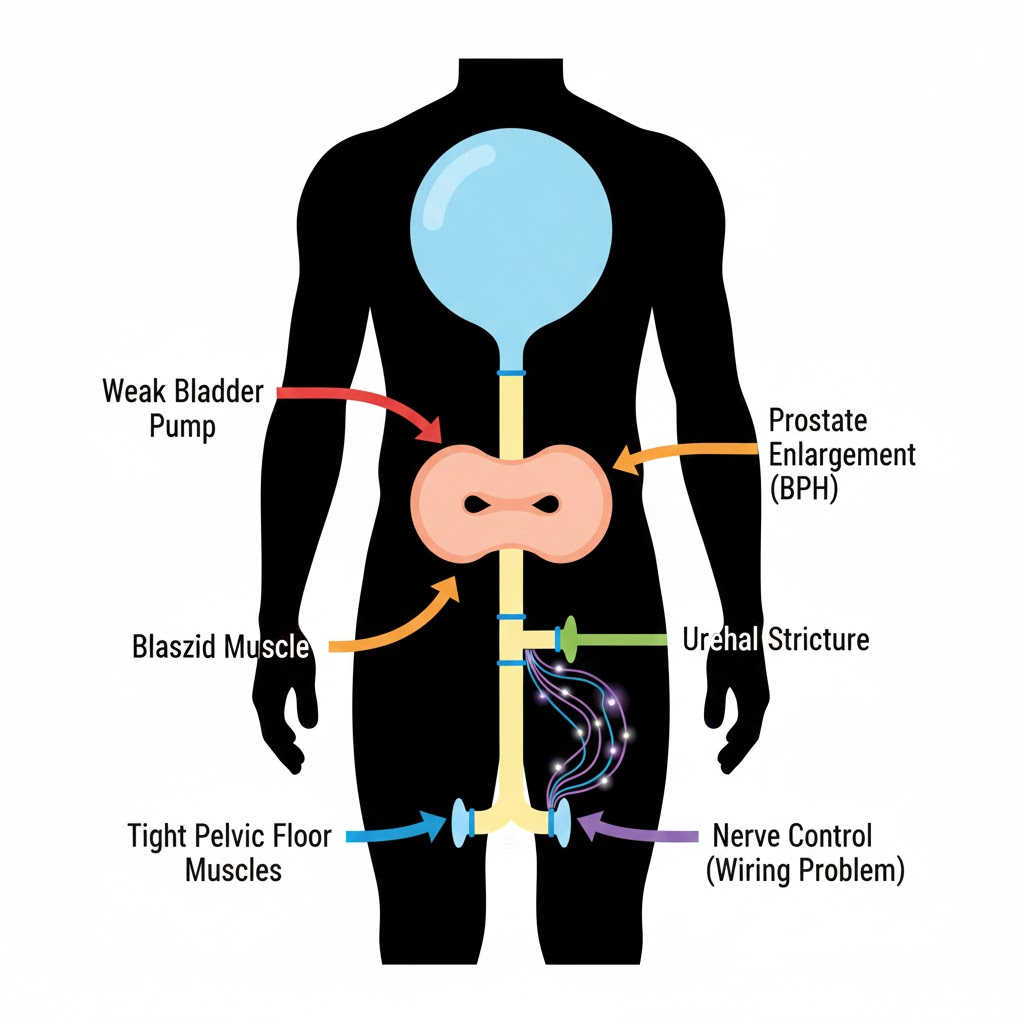
While BPH itself doesn’t directly cause erectile dysfunction (ED), several factors create a perfect storm:
- Shared Blood Supply & Nerves: The prostate, bladder, and erectile tissues share a network of delicate blood vessels and nerves. Inflammation or surgical procedures in the prostate area can affect adjacent structures responsible for erections.
- Nocturia & Fatigue: Chronic sleep disruption from frequent nighttime urination leads to fatigue and low testosterone, both libido killers.
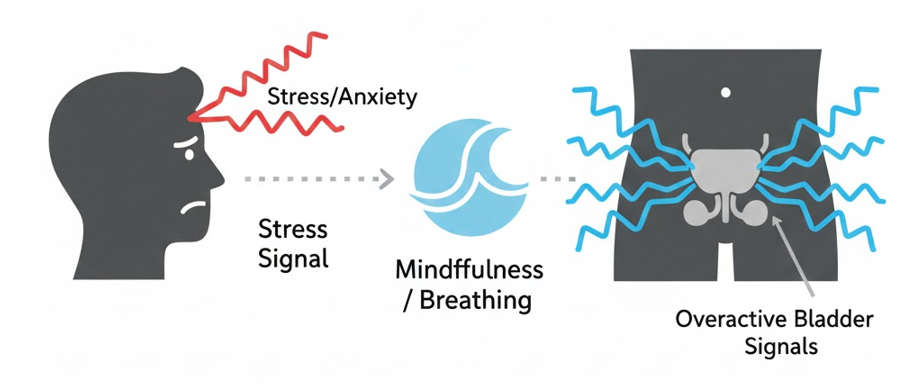
- Psychological Impact: The anxiety and stress of managing a chronic condition, worrying about urinary leaks during sex, or feeling “less masculine” can significantly affect sexual desire and performance.
The Ejaculation Equation
BPH’s effect on ejaculation is often more direct:
- Weaker Ejaculation Force: As the prostate enlarges, it can partially obstruct the ejaculatory ducts.
- Decreased Ejaculate Volume: The prostate produces about 30% of semen volume. An enlarged, dysfunctional prostate may produce less fluid.
- Pain or Discomfort: In some men, particularly those with concurrent inflammation (prostatitis), ejaculation can become painful—a condition known as dysorgasmia.
The Medication Effect: What Your BPH Drugs Do to Your Sex Life
Alpha-Blockers (Flomax, Rapaflo, etc.)
- Erection Impact: Minimal direct effect. However, side effects like dizziness and fatigue can reduce sexual desire.
- Ejaculation Impact: MAJOR. These medications commonly cause retrograde ejaculation (dry orgasm), where semen goes backward into the bladder instead of out. This affects up to 90% of men on tamsulosin or silodosin. It’s harmless but can be psychologically unsettling.
- Management: If retrograde ejaculation is bothersome, discuss switching to alfuzosin, which has a lower incidence, or exploring non-medication options.
5-Alpha Reductase Inhibitors (Finasteride, Dutasteride)
- Erection Impact: Yes. These drugs can cause erectile dysfunction (ED) and decreased libido in ~5-10% of men. The mechanism is related to lowering DHT, a hormone involved in sexual function.
- Ejaculation Impact: May decrease ejaculate volume.
- Important: A small percentage of men report persistent sexual side effects even after stopping the drug (Post-Finasteride Syndrome). Discuss this risk with your doctor.
Tadalafil (Cialis) – The Dual-Purpose Drug
This PDE5 inhibitor is unique—it’s FDA-approved for both BPH and ED. It works by relaxing smooth muscle in the prostate and bladder neck, improving urine flow, and in the penile arteries, improving erections. Learn more in our guide: Tadalafil (Cialis) for BPH: Does it Work?
Surgical Procedures & Sexual Side Effects: What to Expect
Any procedure that alters the prostate anatomy carries sexual side effect risks. The key is informed consent—knowing the trade-offs.
- TURP & Laser Surgeries (GreenLight):
- Retrograde Ejaculation: Very common (75-90%). These procedures reshape the bladder neck, making it near-universal.
- Erectile Dysfunction Risk: ~5-15%. Modern techniques have reduced this risk significantly from older methods.
- Minimally Invasive Therapies (UroLift, Rezūm):
- Key Advantage: These are specifically designed to preserve sexual function.
- UroLift: Does not typically cause retrograde ejaculation (preserves antegrade ejaculation in ~95% of men).
- Rezūm: Also aims to preserve ejaculatory function, though some changes may occur.
For a realistic look at recovery, including the return to sexual activity, see: BPH Surgery Recovery: One Man’s Diary
Strategies to Protect & Enhance Your Sexual Health
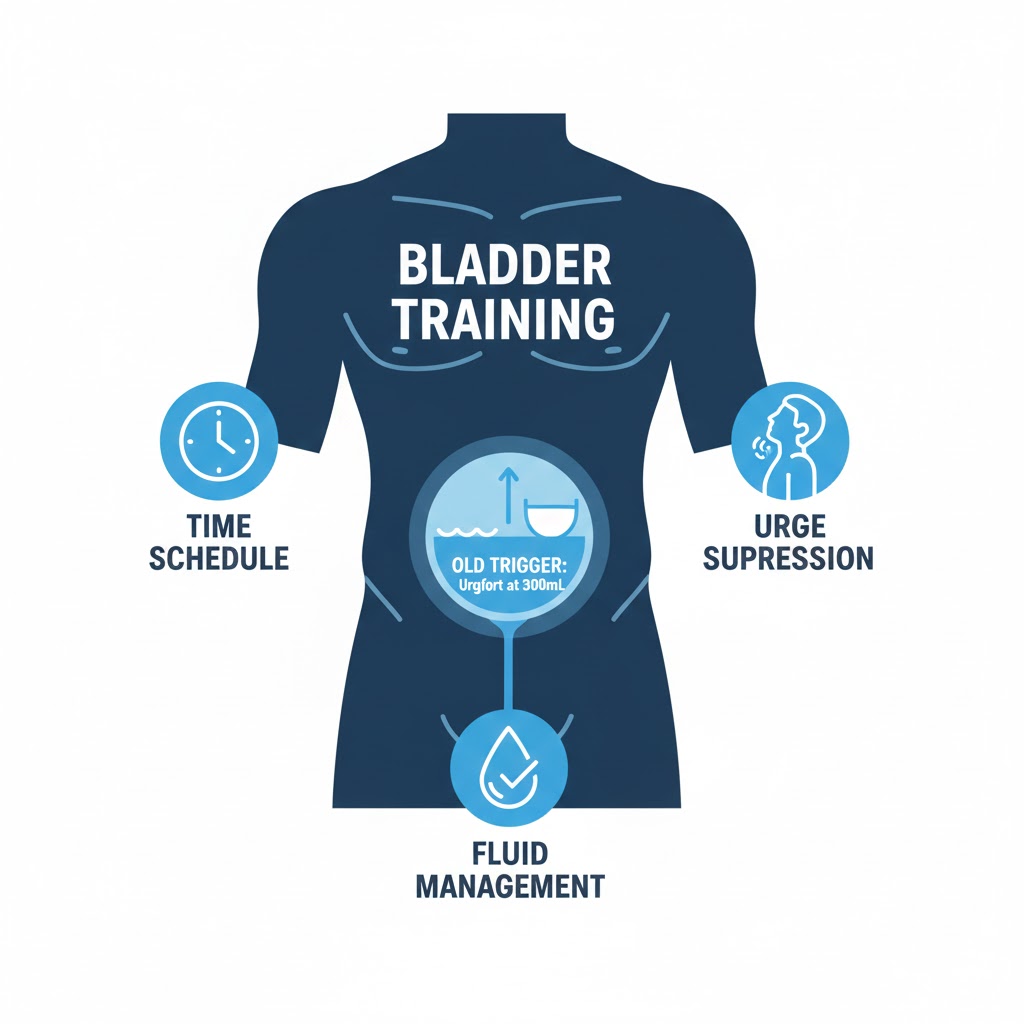
Lifestyle & Natural Approaches
- Pelvic Floor Power: Strong pelvic floor muscles improve erectile rigidity and ejaculatory control. Our Pelvic Floor Exercise Guide is essential.
- Anti-Inflammatory Diet: Reduce systemic inflammation that can affect blood flow. Follow our 7-Day Prostate Health Diet Plan.
- Cardiovascular Exercise: What’s good for your heart is good for erectile function. Aim for 150 minutes of moderate exercise weekly.
- Stress & Sleep Management: Address the psychological side. Techniques from our Stress Management for BPH guide can improve libido.
Communication & Intimacy
- Talk to Your Partner: Share your concerns. Often, the fear is worse than the reality. Focus on intimacy beyond penetration.
- Talk to Your Urologist: Be explicit about your sexual health priorities. Ask: “Which treatment option best preserves my sexual function?”
- Consider Sex Therapy: A therapist can help navigate changes and maintain connection.
Medical Interventions for ED
If ED becomes an issue, numerous effective treatments exist:
- Oral PDE5 Inhibitors: Sildenafil (Viagra), Tadalafil (Cialis), Vardenafil (Levitra).
- Other Options: Vacuum erection devices, penile injections, implants.
- Testosterone Replacement: Only if blood tests confirm low testosterone.
When to Seek Help: Red Flags & Specialist Care
Consult a urologist or sexual health specialist if you experience:
- Persistent inability to get or maintain an erection satisfactory for sex.
- Complete absence of ejaculation (anejaculation) or painful ejaculation.
- Significant, unwanted changes in libido.
- Sexual side effects from medication that severely impact your quality of life.
Remember: Sexual health is an integral part of overall well-being. Your concerns are valid and treatable.
Conclusion: A Balanced Approach to Prostate and Sexual Health
Managing BPH doesn’t mean sacrificing your sex life. It means making informed choices—understanding how different treatments affect sexual function and prioritizing options that align with your personal goals. By addressing both urinary and sexual health proactively, you can find a path that maintains your comfort, function, and intimacy.
Your Action Plan:
- Assess: Which aspect is most affected—libido, erection, or ejaculation?
- Review: List your medications and their potential sexual side effects.
- Discuss: Bring this topic up at your next urologist appointment. Use our Urologist Appointment Prep Guide for support.
- Experiment: With your partner, explore new forms of intimacy that aren’t focused solely on performance.
Navigate Our Complete BPH Hub:
- Silo 1: BPH Symptoms & Daily Management (You are here)
- Silo 2: Medical & Surgical Treatments
- Silo 3: Natural Remedies & Lifestyle
- Main Hub: The Complete Guide to BPH & Prostate Health
FAQs
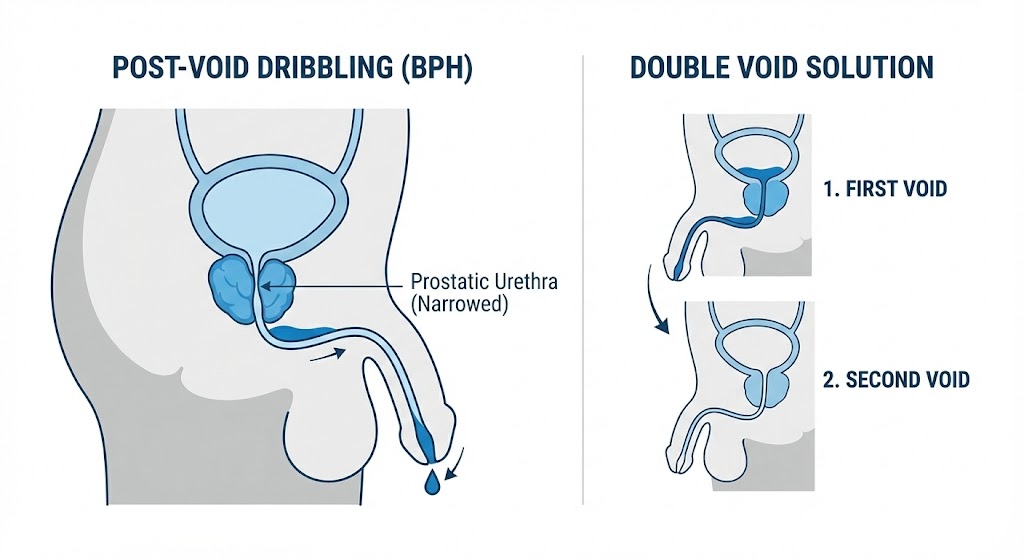
1. Is retrograde ejaculation harmful? Can you still orgasm?
Retrograde ejaculation is not physically harmful. The semen simply empties into the bladder and is later passed with urine (which may look cloudy). Yes, you can still experience orgasm—the pleasurable sensations and muscular contractions of orgasm remain unchanged. The only difference is the absence of semen ejaculation. It can affect fertility, however.
2. Will stopping Flomax bring back normal ejaculation?
In most cases, yes. Retrograde ejaculation caused by alpha-blockers like Flomax is usually reversible within a few days to weeks of stopping the medication. However, if you switch to another BPH medication or undergo surgery, the issue may persist due to the new treatment.
3. Can BPH cause premature ejaculation (PE)?
There’s no direct physiological link, but indirect connections exist. The anxiety and stress of managing BPH symptoms, or the fear of urinary leakage during sex, can lead to performance anxiety, which is a common cause of PE. Additionally, some men may rush sexual activity due to urinary urgency.
4. How soon after BPH surgery (TURP/UroLift) can you have sex?
This varies by procedure and individual healing. Generally, urologists recommend waiting 4-6 weeks after TURP or laser surgery to allow the prostate to heal fully and reduce the risk of bleeding. For minimally invasive procedures like UroLift, the wait may be shorter (2-4 weeks). Always follow your surgeon’s specific instructions.
5. Are there any BPH treatments that DON’T affect sexual function?
Minimally Invasive Therapies are your best bet for preservation. UroLift is specifically designed to not cause retrograde ejaculation. Rezūm also aims to preserve function, though changes can occur. Medications all have some sexual side effect profile, though alfuzosin has lower retrograde ejaculation risk than tamsulosin.
6. Can pelvic floor exercises really help with ED from BPH?
Yes, significantly. Strong pelvic floor muscles (particularly the bulbocavernosus and ischiocavernosus) are crucial for maintaining rigid erections and preventing blood from leaving the penis. Weakness here can contribute to erectile issues. Our Pelvic Floor Exercise Guide targets these muscles.
7. My libido has dropped since starting Finasteride. What can I do?
First, discuss this with your prescribing doctor. Options include: 1) Waiting it out—side effects sometimes diminish after several months. 2) Adjusting the dose (if appropriate). 3) Switching to a different medication class (like an alpha-blocker). 4) Adding a libido-supporting approach like exercise, stress reduction, or (if levels are low) investigating testosterone.
8. What is “post-orgasm urine leakage” and is it related to BPH?
This is different from retrograde ejaculation. Some men experience urine leakage immediately after orgasm, often due to a weak pelvic floor that cannot maintain closure of the bladder neck during the intense contractions of orgasm. This is more related to pelvic floor dysfunction than BPH directly, but the conditions often co-exist. Pelvic floor physiotherapy is the primary treatment.
9. Should I get my testosterone checked if I have BPH and low libido?
Yes, it’s a reasonable request. While BPH itself isn’t caused by low testosterone, the fatigue and metabolic factors associated with BPH can contribute to low T. It’s important to rule out testosterone deficiency as a contributor to low libido. However, testosterone replacement therapy can sometimes worsen BPH symptoms, so this must be managed carefully by a specialist.
10. How do I talk to my partner about these changes?
Be honest and factual, not apologetic. Frame it as a health challenge you’re navigating together. Say something like: “My prostate condition and the treatments for it can affect our sex life in some ways I’m learning about. I’d like us to figure this out together and find what works for us.” Focus on intimacy, not just intercourse.
Related Articles
- Tadalafil (Cialis) for BPH: The Dual-Purpose ED & Urinary Drug: Deep dive into this unique medication option.
- BPH Medication Guide: Alpha-Blockers vs. 5-ARIs Side Effects: Understand the specific sexual side effects of common drugs.
- UroLift vs. TURP: Comparing Sexual Function Outcomes: See how surgical choices impact sexual health.
- The Role of Stress Management in BPH: Learn techniques to reduce anxiety that impacts sexual performance.
Your Journey to Better Prostate Health Starts Here
This article is just one part of our complete, 30+ article resource on BPH and prostate health.
From first symptoms to treatment recovery, natural remedies to surgical deep dives—we’ve covered it all in one place.
🗺️ Explore The Complete BPH & Prostate Health HubInside: Symptom Trackers | Treatment Comparisons | Recovery Diaries | Diet Plans | FAQs | and much more.
Considering a Natural Prostate Supplement?
Many of our readers have asked about comprehensive natural formulas. Prostavive combines 9 research-backed ingredients including Saw Palmetto, Beta-Sitosterol, and Pygeum in one supplement.
Note: The Health Knowledge Base are Trusted Affiliates of Prostavive. We earn a commission if you purchase, at NO EXTRA COST TO YOU. Always consult your healthcare provider before starting supplements.