When Your Mind Affects Your Prostate: The Stress-BPH Connection
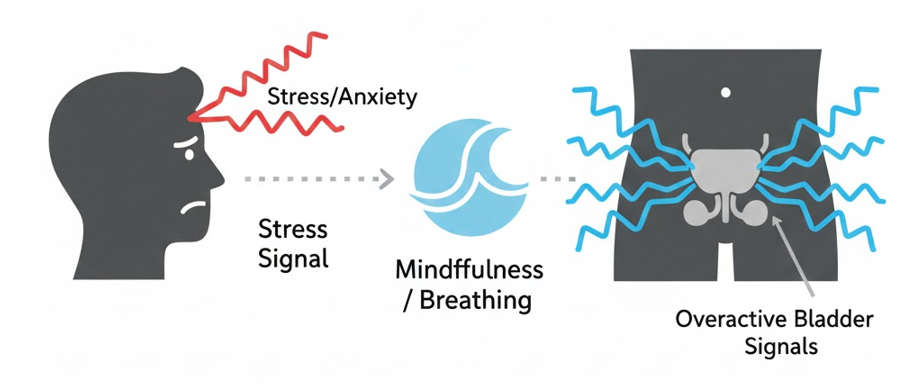
You’ve likely noticed it: during a high-pressure week at work, after a heated argument, or when anxiety is running high, your urinary symptoms seem to intensify. This isn’t imagination—it’s physiology. While stress doesn’t cause BPH, it can significantly worsen symptoms like urgency, frequency, and nocturia, turning manageable symptoms into disruptive flare-ups.
Understanding and managing the mind-body connection is a powerful, often overlooked tool in your BPH management toolkit. This guide explores why stress triggers urinary symptoms and provides practical, evidence-based techniques to calm your nervous system and, in turn, calm your overactive bladder.
The Science: How Stress “Turns Up the Volume” on BPH Symptoms
Stress activates your sympathetic nervous system—the “fight or flight” response. This ancient survival mechanism has several direct effects on your urinary system:
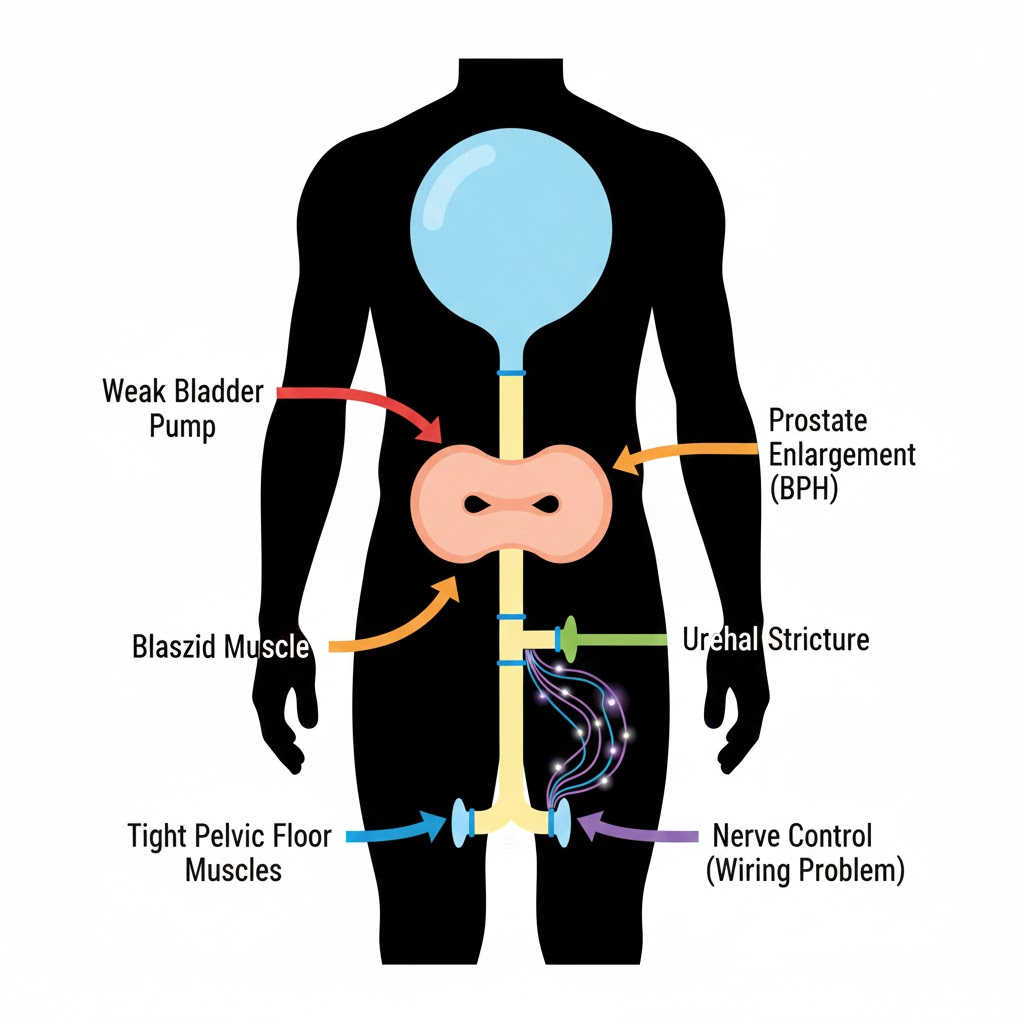
1. Muscle Tension & Pelvic Floor Dysfunction
- The Response: Stress causes involuntary tightening of skeletal muscles, including the pelvic floor.
- The BPH Impact: A tense pelvic floor cannot fully relax during urination, worsening obstructive symptoms (hesitancy, weak stream) and preventing complete emptying. This leads to residual urine and more frequent trips.
2. Bladder Muscle Irritability (Detrusor Overactivity)
- The Response: Stress hormones (cortisol, adrenaline) can make the smooth muscle of the bladder wall (detrusor) more excitable and prone to involuntary contractions.
- The BPH Impact: This directly increases urgency and frequency, the classic “overactive bladder” symptoms that often accompany BPH.
3. Altered Pain Perception & Central Sensitization
- The Response: Chronic stress lowers your pain threshold and can lead to central sensitization, where the nervous system becomes hyper-responsive.
- The BPH Impact: Normal sensations of bladder fullness are amplified into urgent, bothersome signals. Discomfort from prostate pressure is felt more acutely.
4. Behavioral Compounding
- The Cycle: Stress → Drink more coffee/alcohol → Symptoms worsen → Anxiety about symptoms increases → More stress. It’s a vicious cycle.
Recognizing Stress-Induced Flare-Ups: Key Signs
Your flare-up might be stress-related if:
- Symptoms worsen during or after periods of high anxiety or pressure.
- You experience nocturia primarily on nights before important events.
- Urgency strikes suddenly in stressful situations, even if your bladder isn’t full.
- You notice increased pelvic discomfort or “pressure” without a change in fluid intake.
- Symptoms improve noticeably during vacations or relaxed periods.
4 Practical Stress Management Techniques for BPH Relief
Technique 1: Diaphragmatic Breathing (The Instant Calmer)
This is your fastest tool to interrupt the stress-urgency cycle.
How to Do It:
- Sit or lie comfortably. Place one hand on your chest, one on your belly.
- Inhale slowly through your nose for 4 seconds, feeling your belly rise (chest should stay relatively still).
- Hold for 2 seconds.
- Exhale slowly through pursed lips for 6 seconds, feeling your belly fall.
- Repeat for 5-10 cycles.
Use it When: You feel a stress wave coming on, or when you feel urinary urgency starting. It directly activates the parasympathetic nervous system (rest-and-digest), countering the fight-or-flight response.
Technique 2: Progressive Muscle Relaxation (PMR) for Pelvic Release
This specifically targets the muscle tension that worsens BPH symptoms.
The Pelvic-Focused Routine:
- Lie down in a quiet space.
- Starting with your feet, tense each muscle group for 5 seconds, then release for 30 seconds, noticing the difference.
- Pay special attention to your pelvic floor: Gently contract (Kegel) for 5 seconds, then completely let go for 30 seconds, focusing on a feeling of warmth and heaviness in the pelvis.
- Work up through your body: legs, glutes, abdomen, hands, arms, shoulders, face.
Practice: Daily for 10 minutes, or use a shortened version when you feel pelvic tightness.
Technique 3: Mindfulness & Urge Surfing
This changes your relationship with the urgent sensation.
The Practice:
- When urgency strikes, pause. Don’t immediately rush to the bathroom.
- Acknowledge the sensation: “This is a feeling of urgency. It is uncomfortable but not dangerous.”
- Breathe into the sensation. Imagine it as a wave—it will crest and then subside.
- Observe how the intensity changes over 60-90 seconds without acting on it.
- Then calmly walk to the bathroom.
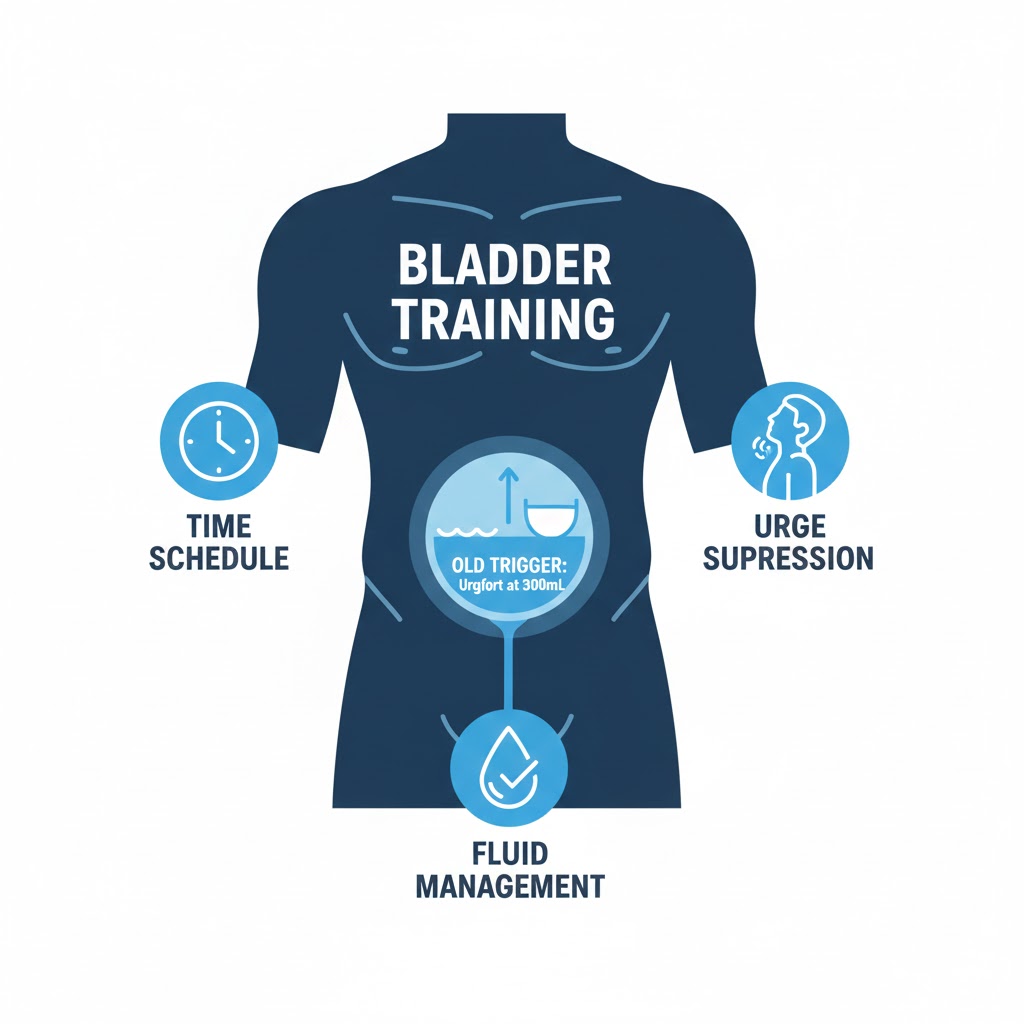
Why it Works: It breaks the conditioned panic response (“URGENCY = EMERGENCY”) and builds confidence that you can tolerate the sensation. Pair this with the skills from our Bladder Retraining Guide.
Technique 4: Scheduled Worry Time & Cognitive Reframing
Prevent all-day anxiety from accumulating.
The Method:
- Set aside 10-15 minutes each day as “worry time.”
- When BPH-related anxieties pop up during the day, jot them on a note and say, “I’ll address this during my worry time.”
- During worry time, review your list. Ask: “Is this thought helpful? Is it true? What’s the evidence?”
- Reframe catastrophic thoughts: Change “I’ll never sleep through the night again” to “I’m learning strategies to improve my sleep, and I had two better nights last week.”
Lifestyle Adjustments to Buffer Against Stress Flare-Ups
Sleep Hygiene for Nocturia Prevention
Poor sleep increases stress hormones. Break the cycle:
- Establish a consistent sleep schedule, even on weekends.
- Implement a “power-down hour” before bed: no screens, dim lights, relaxation.
- If you wake with urgency, practice diaphragmatic breathing in bed for 2 minutes before getting up. You may fall back asleep.
Movement as Medicine
- Regular moderate exercise (walking, swimming) lowers baseline cortisol.
- Avoid prolonged sitting: Set a timer to stand and stretch every 30 minutes to relieve pelvic pressure.
- Gentle yoga or tai chi combines movement with breath awareness, excellent for pelvic relaxation.
Dietary Considerations
- Limit “stress drinking”: Reaching for extra coffee or alcohol when stressed directly irritates the bladder.
- Stay hydrated with water: Dehydration from stress-skipped drinks concentrates urine, increasing irritation.
- Consider adaptogens: Herbs like ashwagandha or rhodiola may help moderate stress response (consult your doctor).
When Stress Management Isn’t Enough: Seeking Professional Help
Consider professional support if:
- Stress is severely impacting your quality of life.
- You have symptoms of clinical anxiety or depression.
- Self-help techniques aren’t providing relief after 4-6 weeks of consistent practice.
Options include:
- Cognitive Behavioral Therapy (CBT): Highly effective for anxiety-related symptom amplification.
- Pelvic Floor Physical Therapy: For stress-related pelvic tension.
- Urologist consultation: To ensure no other medical issue is coinciding.
Creating Your Personal Stress-BPH Action Plan
- Identify Your Triggers: Keep a simple log for a week. Note stress levels (1-10) and symptom severity. Look for patterns.
- Choose Your Primary Technique: Pick one of the four techniques above to practice daily for 2 weeks.
- Build Your Response Plan: Decide what you’ll do at the first sign of a stress flare-up (e.g., 5 cycles of diaphragmatic breathing + urge surfing).
- Measure Progress: Use our BPH Symptom Tracker to see if stress management reduces your IPSS score.
Conclusion: Your Mind is Part of Your Treatment Team
Managing BPH isn’t just about medications, procedures, or even diet and exercise—it’s also about managing your nervous system’s response to the condition. By incorporating stress management into your daily routine, you’re not just “relaxing more”; you’re actively treating the physiological mechanisms that amplify your symptoms.
Remember: Stress doesn’t cause BPH, but calming your stress response can significantly calm your bladder. The goal isn’t a stress-free life (impossible), but a more resilient response that prevents everyday stresses from turning into urinary crises.
Start Small: Tomorrow, practice diaphragmatic breathing for 2 minutes when you wake up. Notice if your first morning urgency is any different. That small experiment is the beginning of reclaiming control.
Navigate Our Complete BPH Hub:
- Silo 1: BPH Symptoms & Daily Management (You are here)
- Silo 2: Medical & Surgical Treatments
- Silo 3: Natural Remedies & Lifestyle
- Main Hub: The Complete Guide to BPH & Prostate Health
FAQs
1. Can stress actually cause BPH (enlarge the prostate)?
No. Stress does not cause the physical growth of prostate tissue that defines BPH. That’s driven by age and hormones (DHT). However, stress can worsen the symptoms of an already enlarged prostate by affecting bladder function, muscle tension, and pain perception. Think of it as stress “turning up the volume” on symptoms, not creating the underlying condition.
2. Why do I feel like I need to pee more when I’m anxious, even if I just went?
This is a classic mind-bladder feedback loop. Anxiety activates your sympathetic nervous system, which can trigger involuntary bladder contractions (detrusor overactivity). Additionally, when anxious, you become hyper-aware of bodily sensations, including normal bladder fullness. The combination creates a powerful, urgent signal that feels immediate even if your bladder isn’t full.
3. Are there specific relaxation techniques better for nighttime symptoms (nocturia)?
Yes. Diaphragmatic breathing in bed is particularly effective. When you wake with the urge to go, try this first: Lie still and take 10 slow, deep belly breaths (4-second inhale, 6-second exhale). Often, the urge will diminish or pass, allowing you to fall back asleep. This breaks the conditioned wake-up response. Also, practice a brief body scan meditation before sleep to release pelvic tension.
4. I have a stressful job. Is it realistic to manage BPH symptoms without changing careers?
Absolutely. The goal isn’t to eliminate stress (impossible), but to change your body’s response to it. Implementing micro-practices throughout your workday can be very effective: 60 seconds of breathing before meetings, setting reminders to stand and stretch (relieving pelvic pressure), staying hydrated with water (not coffee), and using your lunch break for a short walk. These small interventions can significantly buffer the impact of job stress on your symptoms.
5. How long does it take to see improvement in symptoms from stress management?
Some effects can be immediate, like using diaphragmatic breathing to quell a sudden urgency wave. For more sustained reduction in baseline symptom severity, consistent practice for 3-4 weeks is typically needed to see measurable changes in frequency or urgency logs. The nervous system needs time to re-pattern its responses.
6. Can medications for anxiety help BPH symptoms?
This is complex. Some anti-anxiety medications (like certain SSRIs) can have side effects like urinary retention, which could worsen BPH emptying issues. Others might help by reducing overall anxiety, potentially easing symptom perception. Never start or stop psychiatric medication for BPH symptoms without consulting both your urologist and psychiatrist. The risks and benefits must be carefully weighed.
7. Is there a link between stress and prostatitis (CPPS) vs. BPH?
The link is stronger with Chronic Pelvic Pain Syndrome (CPPS, a type of prostatitis), where stress and anxiety are considered major triggers and perpetuating factors. With BPH, stress exacerbates functional symptoms (urgency, frequency) more than it causes the structural enlargement. However, the two conditions can overlap. If you have significant pelvic pain with stress, review our guide on Prostatitis vs. BPH.
8. Will treating my BPH with surgery or medication reduce my stress about it?
Often, yes. Effective treatment that significantly improves symptoms can break the anxiety cycle. Knowing you have a strong stream or can sleep through the night reduces the constant background worry about finding a bathroom or having an accident. However, if you have a pre-existing anxiety disorder, the underlying anxiety may persist and benefit from separate management.
9. Can pelvic floor physical therapy help with stress-related BPH symptoms?
Yes, immensely. A pelvic floor PT can assess if stress is causing you to chronically hold tension in your pelvic muscles, contributing to obstruction and poor emptying. They can teach you specific relaxation and down-training techniques (the opposite of Kegels) that are hard to learn on your own. This is especially valuable if you have a history of “holding stress in your gut.”
10. Are there any quick tips for stressful situations like long car trips or meetings?
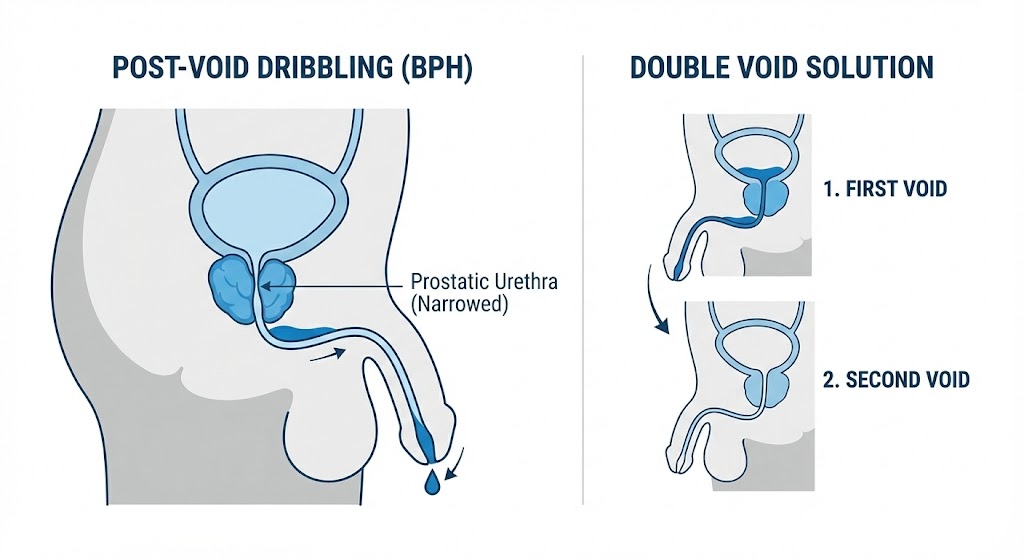
- Pre-emptive Emptying: Double void right before the event.
- Breathing Anchor: Practice discreet diaphragmatic breathing during the event.
- Posture Check: Sit with your knees slightly apart and lean forward slightly to reduce pelvic floor tension.
- Mental Reframe: Remind yourself, “This sensation is uncomfortable but safe. It will pass.”
- Escape Plan: Knowing you can excuse yourself if absolutely necessary (and having a plan) often reduces the anxiety that fuels the urgency.
Related Articles
- Bladder Retraining for BPH: Increase Your Control: Combine stress management with behavioral training for maximum symptom control.
- Pelvic Floor Exercises for BPH: Learn to Relax & Strengthen: Target the specific muscle tension that stress creates.
- Nocturia Fixes: How to Stop Nighttime Bathroom Trips: Apply stress-reduction techniques specifically for better sleep.
- Caffeine & Alcohol Moderation for BPH: Manage the dietary choices often worsened by stress.