For many men, the slow progression of Benign Prostatic Hyperplasia (BPH) symptoms—a slightly weaker stream here, an extra bathroom trip there—feels like a normal part of aging, not an urgent medical issue. This leads to the procrastination trap: “I can just live with it.” However, BPH is rarely static. It is a progressive condition where the prostate typically continues to enlarge over time. Ignoring these symptoms isn’t merely about tolerating inconvenience; it’s about risking significant, sometimes irreversible, damage to your entire urinary system.
Understanding the long-term outlook is crucial. Untreated BPH can evolve from a lifestyle nuisance into a source of serious complications, with Acute Urinary Retention (AUR) representing a sudden and painful tipping point. This guide outlines the real risks of inaction, explaining how the bladder and kidneys pay the price, so you can make informed decisions about your health before a crisis forces your hand.
The “Point of No Return”: Acute Urinary Retention (AUR)
Acute Urinary Retention (AUR) is the sudden, complete, and often excruciating inability to pass urine, despite having a full bladder. It is a urological emergency.
- The ER Reality: AUR requires immediate catheterization in an emergency room to drain the bladder and relieve severe pain and pressure. It’s a stark, frightening introduction to the consequences of untreated BPH.
- Trigger Factors: An already narrowed urethra can be pushed “over the edge” by common triggers:
- Medications: Over-the-counter cold and allergy drugs containing decongestants (pseudoephedrine) or antihistamines, which can tighten the muscles at the bladder neck.
- Alcohol: Acts as a diuretic and a sedative, leading to overfilling and impaired sensation.
- Delayed Voiding: “Holding it” for too long, especially when the bladder is already overworked.
The occurrence of AUR is a major red flag. Studies show that once a man experiences an episode, his likelihood of requiring future surgery increases significantly. For a deeper look at surgical options that may become necessary, see our guide: TURP vs. Laser Surgery (GreenLight): Which BPH Procedure is Right for You?.
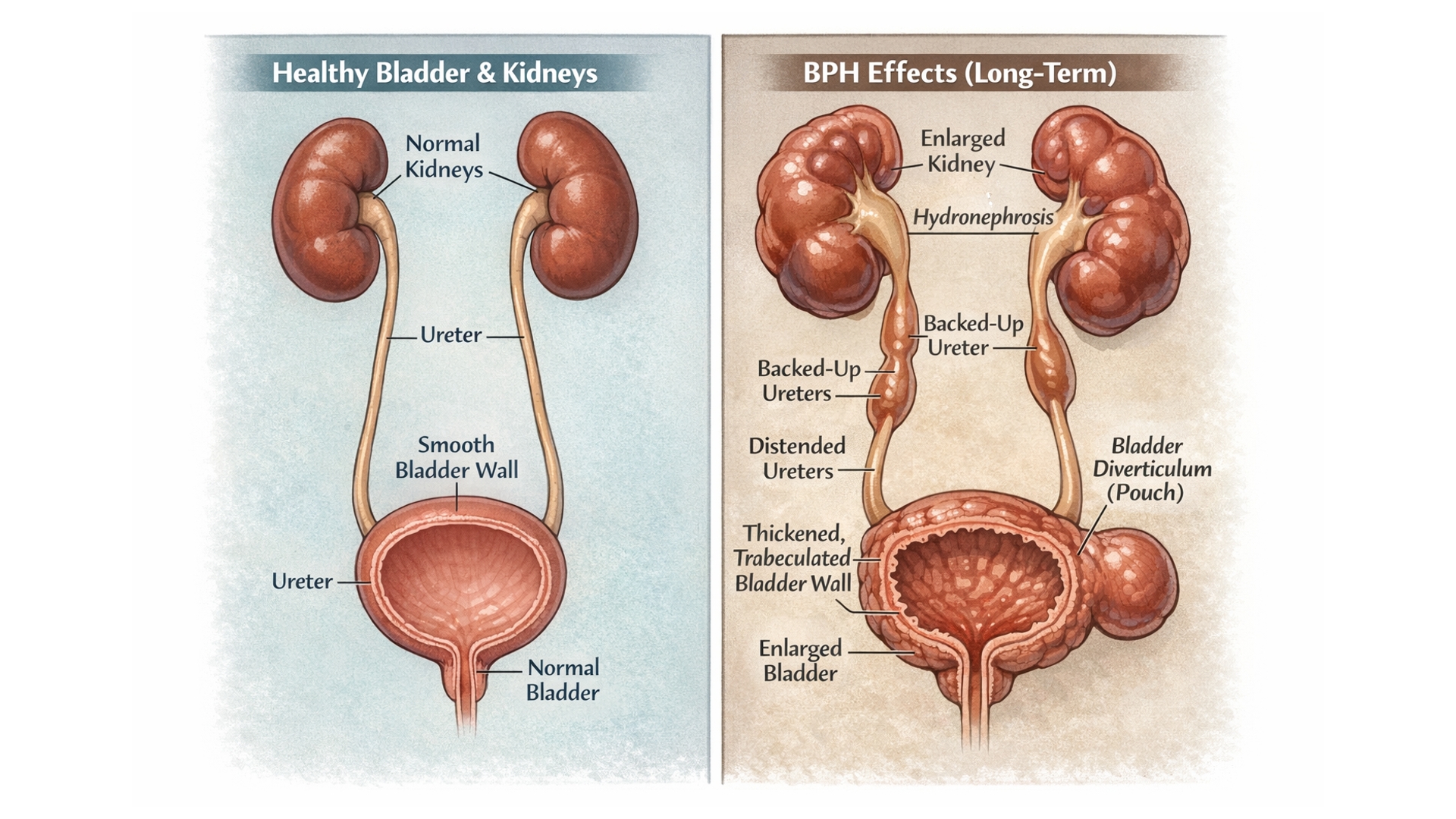
The Bladder’s Breaking Point: From Overworked to Damaged
Your bladder is a muscular sac designed to fill and empty efficiently. Chronic obstruction from BPH forces it to work against a constant resistance, leading to structural damage over years.
- Bladder Wall Thickening (Trabeculation): To force urine past the obstruction, the bladder muscle hypertrophies, becoming thick, scarred, and less elastic. Imagine a over-exercised, knotted muscle that can’t relax properly.
- Diverticula: High pressure can cause weak spots in the bladder wall to balloon outward, forming pouches. These diverticula trap urine that doesn’t empty, leading to infection and stone formation.
- The “Decompensated” Bladder: In severe, long-standing cases, the overworked muscle fibers fail and are replaced by scar tissue. The bladder loses its ability to contract effectively, becoming a floppy, atomic sac. This is the tragic scenario where a man may still be unable to urinate normally even after a successful prostate surgery because the bladder itself is beyond repair.
Collateral Damage: Kidneys and Chronic Infections
The damage doesn’t stop at the bladder. A compromised lower urinary tract can have upstream consequences.
- Hydronephrosis: Persistent high pressure can cause urine to reflux back up the ureters into the kidneys. This back-pressure swells and damages the delicate kidney structures, potentially leading to permanent kidney failure if left unaddressed.
- Chronic Urinary Tract Infections (UTIs): Incomplete emptying creates stagnant urine, which is a perfect breeding ground for bacteria. Recurrent infections cause pain, fever, and can further scar the bladder.
- Bladder Stones: Minerals in urine crystallize over time. In a bladder that doesn’t empty fully, these crystals can grow into large, painful stones that irritate the lining, cause bleeding, and harbor infection.
When “Watchful Waiting” Becomes Risky Inaction
It’s vital to distinguish between “Watchful Waiting”—a valid, medically supervised strategy for mild, non-bothersome symptoms—and ignoring the problem. Under watchful waiting, a doctor monitors you for the very red flags that indicate it’s time to intervene.
Key Red Flags That Demand Action:
- Recurrent Hematuria: Blood in the urine, visible or microscopic, indicating irritation or stones.
- Overflow Incontinence: Frequent dribbling or leakage because the bladder is chronically overfull and simply spills over.
- Disruptive Nocturia: Waking up multiple times a night to urinate, severely fragmenting sleep and impacting overall health. For strategies on managing this symptom, see: Nocturia Fixes: How to Stop Nighttime Bathroom Trips.
- Acute or Frequent UTIs.
If you are under a urologist’s care and tracking symptoms, you are not “untreated.” To learn more about this monitored approach, read: The Watchful Waiting Approach for Mild BPH.
The Proactive Path: Preservation Over Repair
The core message is one of prevention. Managing BPH proactively is fundamentally about preserving the health and function of your bladder and kidneys. It is far easier—and more effective—to maintain a healthy organ through timely treatment than to attempt repairing one that has been damaged by years of silent obstruction.
Proactive management also brings profound peace of mind, freeing you from the constant anxiety of locating bathrooms, fearing embarrassing leaks, or dreading a sudden, painful retention event.
Conclusion: Your Symptoms Are a “Check Engine” Light
The urinary symptoms of BPH are not just annoyances; they are your body’s persistent “check engine” light for the entire urinary system. Ignoring them risks progressive, costly, and potentially irreversible damage.
The goal is not to incite fear, but to empower with knowledge. Understanding these risks provides the strongest possible motivation to take a proactive step. That step begins with a informed conversation with a healthcare professional.
Ready to start that conversation but unsure what to ask? Arm yourself with the right questions to take control of your health journey.
✅ FAQs
Q1: Can BPH actually kill you?
A: While BPH itself is not directly fatal, its complications can be life-threatening. Severe kidney damage (renal failure) from long-term obstruction or urosepsis (a bloodstream infection originating from a urinary tract infection) are serious medical emergencies that can lead to death if not treated promptly.
Q2: How common is acute urinary retention (AUR)?
A: The risk increases with age and symptom severity. For men in their 70s with moderate to severe BPH symptoms, the lifetime risk of experiencing an episode of AUR is estimated to be as high as 10-15%. The risk is much lower with proactive management.
Q3: What does “overflow incontinence” feel like?
A: It often feels like a constant, uncontrollable dribbling of small amounts of urine, rather than a large gush. This happens because the bladder is so full and stretched that it simply leaks urine around the obstruction. There is no sensation of a strong urge to go.
Q4: Can kidney damage from BPH be reversed?
A: It depends on the severity and duration. Mild to moderate hydronephrosis (kidney swelling) often improves significantly once the bladder obstruction is relieved. However, long-term, high-pressure obstruction can cause irreversible scarring (renal fibrosis). This underscores the importance of early intervention.
Q5: I have mild symptoms. Should I be worried about these risks?
A: The risks outlined are primarily associated with moderate to severe, untreated BPH over many years. If your symptoms are mild and stable under a doctor’s “watchful waiting” plan, your risk is low. The key is regular monitoring to catch progression early. Track your symptoms: BPH Self-Assessment: Quizzes and Tools.
Q6: If I have AUR once, will it happen again?
A: The risk of recurrence is high. After a first episode of AUR (often treated with a temporary catheter), there is a significant likelihood it will happen again unless the underlying obstruction is addressed with medication or a procedure.
Q7: Are bladder stones a common complication?
A: They are a well-known complication of long-standing, incomplete bladder emptying. While not everyone with BPH will develop them, the stagnant urine environment significantly increases the risk. Stones can cause pain, bleeding, and recurrent infections.
Q8: Can lifestyle changes prevent these severe complications?
A: Lifestyle changes (fluid management, diet, avoiding triggers) are excellent for managing symptoms and improving quality of life, and may slow progression. However, they cannot reverse anatomical obstruction or reliably prevent complications like AUR or kidney damage in a significantly enlarged prostate. Medical treatment is required for that.
Q9: What’s the difference between an overactive bladder (OAB) and a decompensated bladder?
A: They are opposites. OAB is a hyperactive, spastic bladder that contracts too often and without warning, causing urgency. A decompensated bladder is a failed, floppy muscle that has lost its contractile power and cannot empty properly. Both can co-exist with BPH, but decompensation is a direct result of long-term obstruction.
Q10: My father had kidney failure. Does having BPH put me at higher risk?
A: It can. If you have a family history of kidney issues, it is even more critical to protect your kidney function. Proactively managing BPH to prevent obstruction-related back-pressure (hydronephrosis) is an important part of preserving your renal health. Discuss this family history with your urologist.
Don’t Wait for a Crisis to Act
Understanding the risks is the first step. The next is exploring your treatment options. Discover the full range of medical and surgical solutions to protect your long-term health.
Explore All BPH Treatments →Ready to Talk to a Doctor? Be Prepared.
If this guide has motivated you to take action, ensure your urologist appointment is productive. Get our list of essential questions and a printable checklist to advocate for your health.
Prepare for Your Urologist Visit →Not Sure How Severe Your Symptoms Are?
Knowledge starts with tracking. Use our official symptom score quiz and bladder diary tool to objectively assess your BPH severity before seeing a doctor.
Take the BPH Symptom Quiz →✅ Related Articles
Understanding BPH & Symptoms:
- BPH Self-Assessment: Quizzes and Tools to Track Your Symptoms at Home: The first step in understanding your personal risk level.
- Weak Urine Stream? 5 Causes Beyond BPH: Rule out other potential causes of urinary symptoms.
Treatment Pathways & Decision-Making:
- The Watchful Waiting Approach for Mild BPH: Criteria and Monitoring: Learn the correct, supervised way to monitor mild symptoms without risking the complications outlined here.
- Preparing for Your Urologist Appointment: 10 Key Questions to Ask: The essential next-step article after reading about risks.
- BPH Surgery Recovery: One Man’s Diary (With Photos): A candid look at recovery from a major procedure, underscoring the benefit of earlier, less invasive intervention.
Managing Specific Complications:
- Nocturia Fixes: How to Stop Nighttime Bathroom Trips (BPH Edition): Targeted strategies for one of the most disruptive symptoms and a key red flag.
- BPH Catheterization: Types, Care, and Preventing Infection at Home: Practical information that becomes relevant if complications like retention occur.