Managing a chronic lung condition like asthma or COPD can feel like a constant guessing game. Is that cough just a tickle, or the start of a flare-up? Is your shortness of breath normal, or a sign you need to adjust your treatment?
The uncertainty ends when you have data.
While nothing replaces a doctor’s expertise, at-home lung monitoring empowers you to move from guessing to knowing. By tracking key metrics, you can spot trends early, understand your triggers, and have more productive conversations with your healthcare team.
This guide walks you through the five most effective tools for monitoring your respiratory health from home, helping you take a proactive role in the journey we outline in our Ultimate Guide to Clearing Mucus & Restoring Lung Health Naturally.
Why Bother with At-Home Monitoring?
- Catch Flare-Ups Early: A downward trend in your numbers can be an early warning sign, allowing you to act before a minor issue becomes a major crisis.
- Track Your Progress: See what’s working. Did starting a new natural remedy for COPD improve your numbers? Data doesn’t lie.
- Reduce Anxiety: Seeing a concrete, normal number can provide reassurance when you feel short of breath, helping to break the fear-shortness cycle.
- Empower Your Doctor’s Visits: Walk in with a log of your data instead of relying on memory. This provides your doctor with invaluable, objective information to optimize your treatment plan.
The 5 Essential At-Home Lung Monitoring Tools
1. Pulse Oximeter: Your Oxygen Gauge
- What it Measures: Blood oxygen saturation (SpO2) and heart rate.
- What the Numbers Mean:
- SpO2: A normal reading is typically 95% to 100%. Consistently reading below 92% is a sign to call your doctor. (For a deep dive, see our guide on pulse oximetry numbers).
- Heart Rate: Can indicate stress on your body; often elevated during a breathing flare-up.
- Best For: Anyone with a chronic lung condition. It’s your quick check to see if your body is getting enough oxygen.
- Pro Tip: Take readings at rest and after activity. Sit still, and ensure your hand is warm for the most accurate result.
2. Peak Flow Meter: Your Asthma Early-Warning System
- What it Measures: Peak Expiratory Flow (PEF)—the maximum speed you can blow air out of your lungs.
- What the Numbers Mean: It helps establish your personal “zones.”
- Green Zone (80-100% of your personal best): Good control.
- Yellow Zone (50-80%): Caution. Your airways are narrowing.
- Red Zone (Below 50%): Medical alert. Use your rescue inhaler and seek help.
- Best For: Primarily for asthma patients to monitor day-to-day changes and response to medication.
- Pro Tip: Your “personal best” is key. Track your peak flow over two weeks when you feel good to establish your baseline.
3. Handheld Spirometer: Your Personal Lung Function Lab
- What it Measures: Key spirometry values like FEV1 (volume exhaled in 1 second) and FVC (total volume exhaled). This is the at-home version of the test we explain in How to Read Your Spirometry Results.
- What the Numbers Mean:
- FEV1: Your most important number for tracking obstructive diseases like COPD. A decline can signal a flare-up.
- FVC: Helps monitor total lung capacity.
- Best For: COPD patients or anyone wanting more detailed data than a peak flow meter provides.
- Pro Tip: Consistency is everything. Use it at the same time each day, before taking your medications, for the most comparable results.
4. Symptom & Trigger Journal: The Big Picture Connector
- What it Measures: This isn’t a device, but a practice. Track your daily symptoms (cough, mucus, shortness of breath), activity level, diet, and environmental factors.
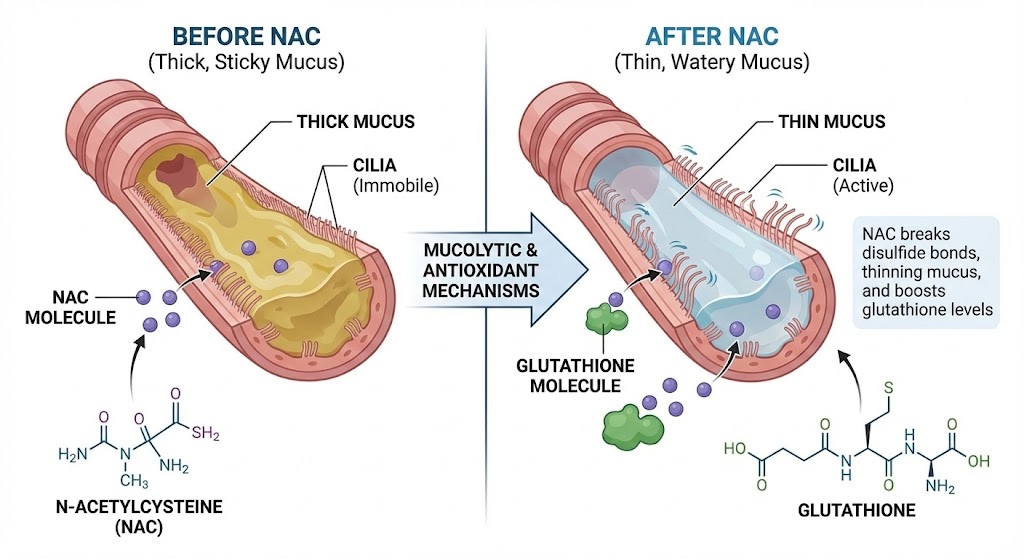
- What the Numbers Mean: You’ll start to see patterns. Do your numbers drop after exposure to a specific indoor toxin or allergen? Does your mucus increase after eating certain foods?
- Best For: Everyone. Connecting quantitative data (numbers) with qualitative data (how you feel) is powerful.
- Pro Tip: Use a simple notebook or a notes app on your phone. Note the date, time, your numbers from other devices, and a brief note on symptoms and potential triggers.
5. Smart Wearable (Fitness Tracker/Smartwatch): Your 24/7 Activity & Breath Coach
- What it Measures: Heart rate, heart rate variability, activity levels, and some advanced models now estimate blood oxygen (SpO2) and even track breathing rate during sleep.
- What the Numbers Mean:
- Resting Heart Rate: A gradual increase can indicate inflammation or that your body is working harder to breathe.
- Activity Tracking: Helps you ensure you’re staying active without overdoing it.
- Best For: Motivation and tracking overall wellness trends. The sleep and activity data is invaluable.
- Pro Tip: Don’t get bogged down in minute-by-minute data. Look for long-term trends over weeks and months.
Creating Your Personalized Monitoring Routine
You don’t need all five tools. Here’s how to choose:
- For Asthma: Peak Flow Meter + Symptom Journal are your essentials.
- For COPD: Pulse Oximeter + Handheld Spirometer + Symptom Journal provide the most comprehensive picture.
- For General Wellness & Anxiety: Pulse Oximeter + Smart Wearable can provide excellent feedback and reassurance.
Sample Morning Routine:
- Upon waking, sit quietly for 5 minutes.
- Take your pulse oximeter reading.
- Perform your peak flow or spirometer test (before breakfast and medication).
- Jot down in your symptom journal how you slept and how you feel.
- Put on your wearable tracker for the day.
Conclusion: You Are the CEO of Your Lung Health
Your doctor is a vital consultant, but you are the one living in your body every day. These at-home monitoring tools put you in the driver’s seat, giving you the data you need to make informed decisions.
Start with one or two tools that resonate with your condition. Track consistently. Watch for trends. This proactive approach is the ultimate strategy for staying ahead of your lung health and achieving the lasting results we champion in our pillar guide to lung health.
FAQs
1. How often should I use my peak flow meter?
If your asthma is stable, once a day (usually in the morning before taking your medication) is sufficient. If you’re in the yellow zone or feeling symptoms, check it 2-3 times a day to monitor your response to medication.
2. Are home spirometers as accurate as the ones in the doctor’s office?
They are generally very good for tracking trends, which is their primary purpose at home. However, the clinical-grade spirometers in a pulmonary function lab are more precise and calibrated regularly. Use your home device to see if your numbers are going up or down, and bring that data to your doctor for interpretation.
3. Can a pulse oximeter detect a COPD flare-up?
Yes, it can be a key indicator. A drop in your normal SpO2 reading (e.g., from 96% to 91%) at rest or with less exertion than usual can be an early sign of a flare-up (or exacerbation), signaling that you should contact your doctor.
4. What’s the most important tool for someone with COPD?
The pulse oximeter is arguably the most critical for daily safety checks, as it directly measures oxygen levels. However, a handheld spirometer provides the best data for tracking the progression of the disease and the effectiveness of your treatment plan over time.
5. Do I need a prescription to buy these tools?
No, all the tools mentioned (pulse oximeters, peak flow meters, consumer-grade handheld spirometers, wearables) are available for purchase over-the-counter without a prescription.
6. How do I find my “personal best” on a peak flow meter?
To find your personal best, use your peak flow meter twice a day for 2-3 weeks when your asthma is under good control. The highest number you achieve during this period is your personal best. This becomes the benchmark for your green, yellow, and red zones.
7. Can tracking my symptoms really make a difference?
Absolutely. A symptom journal helps you connect the dots between your environment, activities, and how you feel. You might discover that your wheezing after walking is worse on high-pollen days, or that certain foods increase mucus, allowing you to avoid those triggers.
8. What should I do if my numbers suddenly drop?
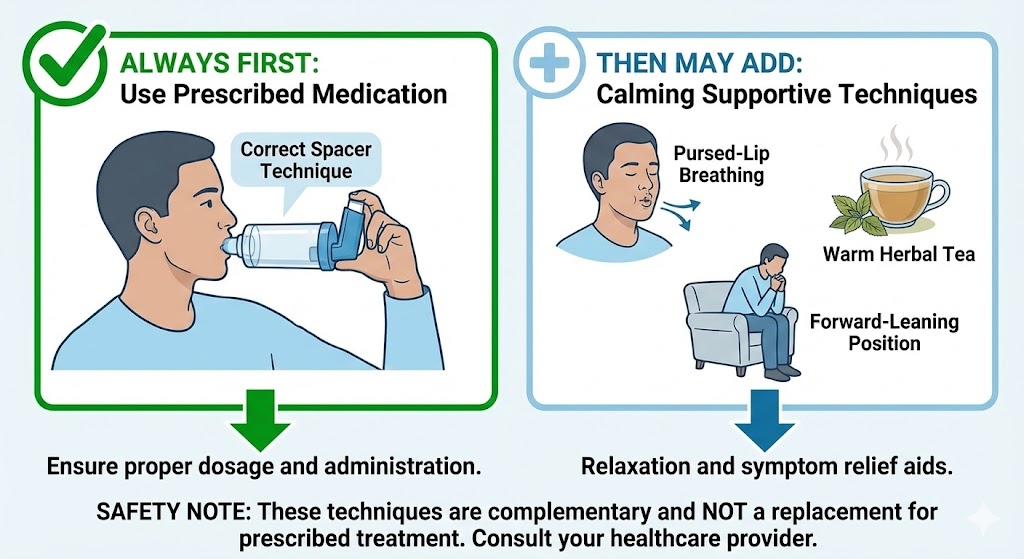
Follow the action plan you’ve created with your doctor. This typically means: 1) Using your rescue medication as prescribed, 2) Resting and re-checking your numbers in 15-20 minutes. If they do not return to your safe (green) zone, or if you have severe shortness of breath, seek medical attention immediately.
9. Is a fitness tracker worth it for lung health?
For motivation and overall health context, yes. Seeing a trend of improved resting heart rate or being able to walk further without your oxygen levels dropping can be incredibly motivating. It helps you see the positive impact of lifestyle changes on your daily lung maintenance.
10. How do I talk to my doctor about my at-home data?
Bring a printed log or your device to your appointment. Say something like, “I’ve been tracking my FEV1 at home, and I noticed it drops by about 10% on days I do yard work,” or “Here’s a log of my morning SpO2 readings for the past month.” This provides concrete evidence to guide your treatment.
Still Have Questions? We Have Answers.
Lung health is complex. If you’re wondering “What about…?” or “What’s next for me?”, you’re not alone. Our Resource Hub is built to be your **first stop for trustworthy, in-depth answers** on every aspect of respiratory wellness.
- Condition-Specific Guides (COPD, Asthma, Post-COVID)
- Step-by-Step Detox & Recovery Plans
- Science-Backed Natural & Conventional Strategies