The Asthma Misdiagnosis Epidemic
You’ve been carrying that inhaler for years, but it barely helps. The wheezing continues, the chest tightness persists, and you’ve started avoiding activities you once loved.
What if you’ve been treating the wrong condition entirely?
Groundbreaking research from the Journal of the American Medical Association reveals that up to 33% of adults diagnosed with asthma don’t actually have it. Many are actually dealing with chronic throat clearing from undiagnosed conditions. Even more shocking? Many are suffering from completely treatable conditions that mimic asthma symptoms.
This isn’t just about misdiagnosis—it’s about getting the right treatment for what’s actually causing your breathing struggles.
The 5 Conditions Most Commonly Mistaken for Asthma
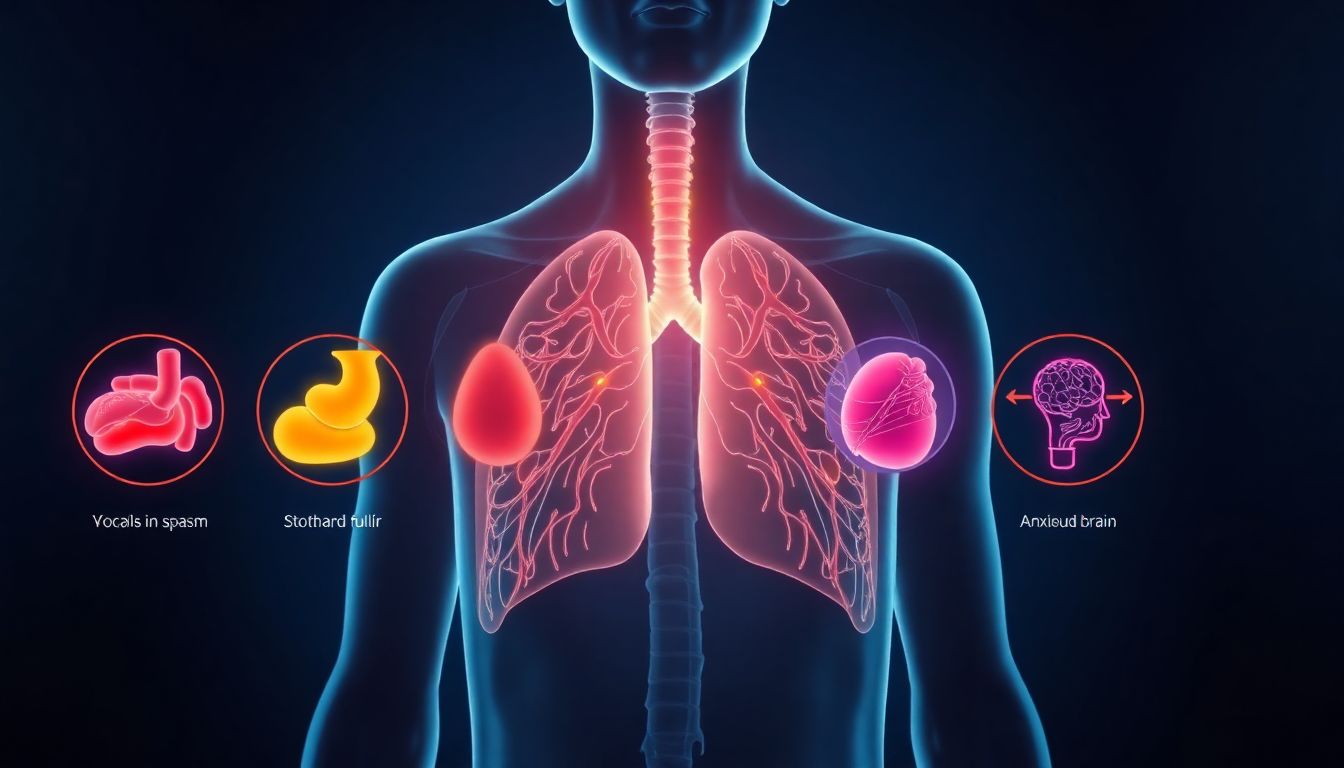
1. Vocal Cord Dysfunction (VCD): The “Asthma Twin”.
(Learn about other surprising causes of wheezing and breathing difficulties.)
What it is: Your vocal cords suddenly close when you inhale instead of opening, creating an asthma-like attack.
Why doctors miss it: The wheezing and stridor sound identical to asthma on superficial examination.
Key differences from asthma:
- Symptoms occur during inhalation (asthma usually during exhalation)
- Rapid onset and resolution
- No response to albuterol. If your medications aren’t working, discover the #1 mistake lung patients make
- Often triggered by stress, strong odors, or exercise
“My inhaler did nothing. Turns out my vocal cords were spasming shut every time I smelled perfume.” — Sarah, 38
2. GERD (Silent Reflux): The Gut-Lung Connection
(Explore how your digestive health affects your breathing in The Gut-Lung Connection.)
What it is: Stomach acid creeping up your esophagus and spilling into airways, causing inflammation and bronchospasms.
Why doctors miss it: You might not feel heartburn—60% of GERD cases are “silent.”
Key differences from asthma:
- Symptoms worsen after meals or when lying down
- Chronic throat clearing and hoarse voice. If you’re constantly clearing your throat, read ‘Why Am I Always Clearing My Throat?’ (Not Allergies)
- Better response to antacids than inhalers
- Often accompanied by post-nasal drip
3. Cardiac Asthma: When Your Heart Mimics Your Lungs
What it is: Heart failure causing fluid buildup in lungs, creating wheezing and shortness of breath.
Why doctors miss it: The symptoms are virtually identical to respiratory asthma.
Key differences from asthma:
- Swelling in ankles and legs
- Symptoms worsen when lying flat
- Fatigue and inability to exercise
- No personal or family history of asthma/allergies
4. COPD Overlap: The Smoker’s Misdiagnosis
(Discover natural approaches in ‘Natural Remedies for COPD: A Science-Backed Approach’)
What it is: Chronic Obstructive Pulmonary Disease often starts with asthma-like symptoms but progresses differently.
Why doctors miss it: Early-stage COPD is frequently mislabeled as “adult-onset asthma.”
Key differences from asthma:
- Progressive rather than episodic
- Minimal reversibility with bronchodilators
- More constant symptoms versus asthma’s attacks
- Strong smoking history (usually 10+ years). See how one man reversed damage in How a 50-Year Smoker Healed His Lungs in 90 Days
5. Anxiety-Induced Breathing Patterns
(Learn calming techniques in Diaphragmatic Breathing: The #1 Exercise to Strengthen Your Lungs & Calm Your Mind.)
What it is: Hyperventilation and dysfunctional breathing patterns that create asthma-like sensations.
Why doctors miss it: The physical symptoms feel so real that both patient and doctor assume it’s asthma.
Key differences from asthma:
- Tingling in fingers and lips
- Feeling of “not getting enough air” rather than wheezing
- Symptoms improve with distraction or relaxation
- No abnormal lung sounds during attacks
Quick Comparison Table: Asthma vs. Imposters
| Condition | Key Differentiating Symptom | Response to Inhaler | Best Diagnostic Test |
|---|---|---|---|
| True Asthma | Wheezing on exhalation | Strong improvement | Spirometry with reversibility |
| VCD | Strider on inhalation | No improvement | Laryngoscopy |
| GERD | Worsens after meals | Minimal improvement | pH monitoring |
| Cardiac | Ankle swelling + SOB | No improvement | Echocardiogram |
| COPD | Progressive SOB | Partial improvement | CT scan + spirometry |
| Anxiety | Tingling + air hunger | No improvement | Breathing pattern assessment |
The 3 Critical Questions Your Doctor Should Ask
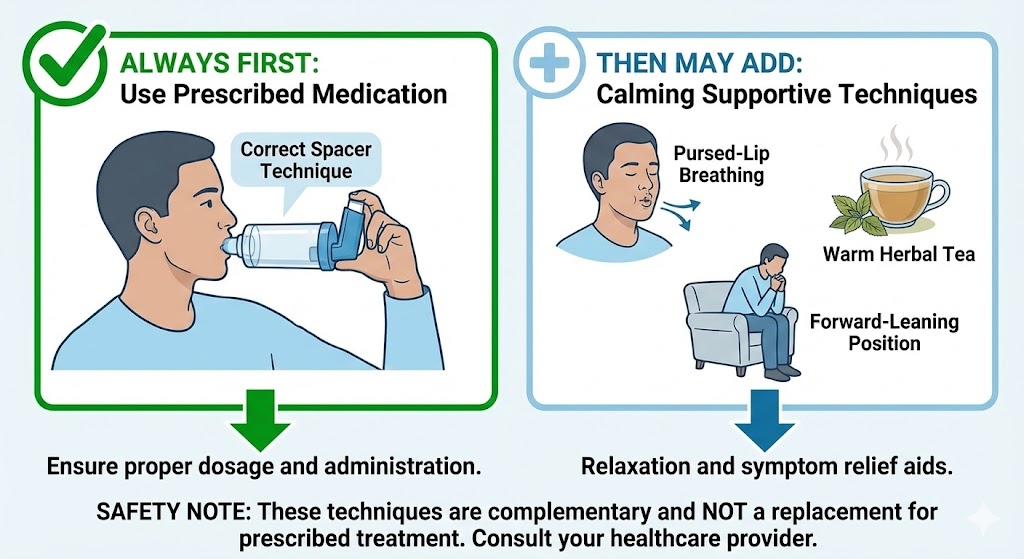
- “Does your inhaler provide immediate, dramatic relief?” (If not, probably not asthma)
- “Do symptoms occur during inhalation or exhalation?” (Inhalation suggests VCD)
- “Is your shortness of breath constant or episodic?” (Constant suggests COPD or cardiac)
FAQs: Your Asthma Misdiagnosis Questions Answered
Q: Can I have both asthma and one of these conditions?
A: Absolutely. Many people have asthma PLUS VCD or GERD, which is why treatment fails—you’re only addressing part of the problem.
Q: How long should I try asthma treatment before seeking a second opinion?
A: If you see no meaningful improvement after 3 months of appropriate asthma therapy, demand further testing.
Q: What’s the most accurate test to confirm or rule out asthma?
A: Spirometry with bronchodilator response is the gold standard. If your doctor hasn’t done this, request it. Get answers to all your lung health questions in Lung Health: 50 Common Questions Answered
Q: Are there natural ways to manage these conditions while I seek diagnosis?
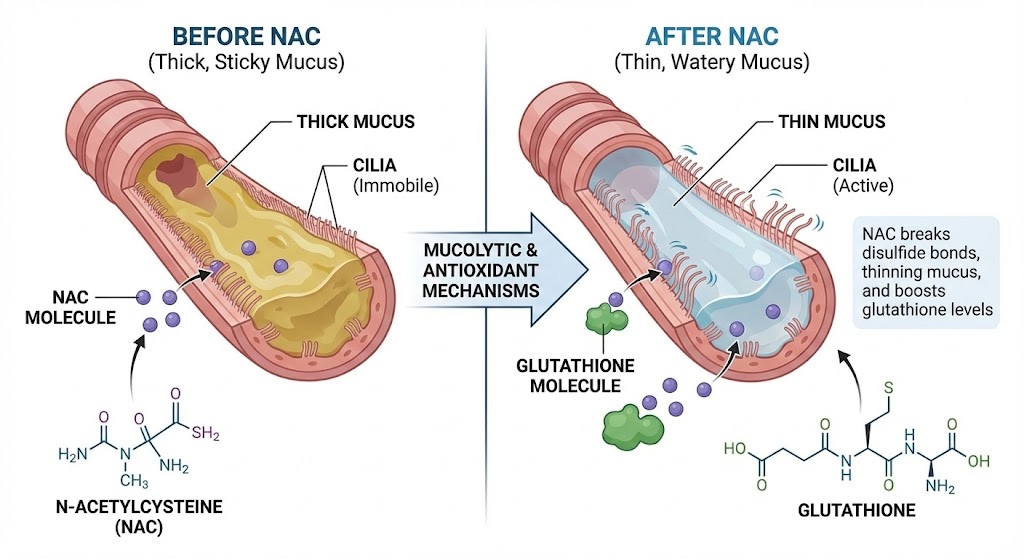
A: Yes. Our Breathe lung drops can help calm airway inflammation regardless of the underlying cause. Learn about the key ingredient in Mullein for Lungs: The Ancient Herb That Melts Mucus
Q: Can stress or anxiety really cause asthma-like symptoms?
A: Absolutely. Stress triggers the “fight or flight” response, causing rapid, shallow breathing that can mimic asthma. The key difference is that anxiety-induced breathing issues typically lack the wheezing sound and respond better to relaxation techniques than inhalers. Many patients find their “asthma” disappears when they address underlying anxiety.
Q: I’ve had asthma since childhood – could it still be a misdiagnosis?
A: While less common, childhood misdiagnoses do occur. Many children outgrow asthma, so if you’re still experiencing symptoms as an adult despite treatment, it’s worth reinvestigating. Conditions like VCD or allergies can persist and be mistaken for lifelong asthma.
Q: How much does proper testing cost if my insurance doesn’t cover it?
A: Basic spirometry costs $150-300, while full pulmonary function tests range from $300-800. Laryngoscopy for VCD detection is $400-1,200. Many clinics offer payment plans, and some university medical centers provide sliding scale fees. Consider it an investment – years of incorrect treatment often cost more in the long run.
Q: Are there specific questions I should ask my pulmonologist during my appointment?
A: Yes, come prepared with:
- “What specific tests will confirm or rule out asthma?”
- “Could my symptoms indicate VCD, GERD, or cardiac issues instead?”
- “If inhalers aren’t helping, what’s our next diagnostic step?”
- “Can you refer me for specialized testing if needed?”
Q: I’m using my inhaler 3-4 times daily but still struggling – is this normal for asthma?
A: No, this indicates poorly controlled symptoms or potential misdiagnosis. Well-managed asthma should require rescue inhalers no more than 2 times weekly. Frequent inhaler use warrants immediate reevaluation of both diagnosis and treatment plan. Discover why some treatments backfire in Why Your Inhaler Makes Your Lung Problems Worse.
Conclusion: Your Path to Proper Diagnosis
Don’t spend another year gasping for air with an ineffective inhaler. The solution starts with asking the right questions and demanding proper testing.
Your 3-Step Action Plan:
- Track your symptoms for 2 weeks—note triggers, timing, and what actually helps
- Request spirometry testing if you haven’t had it
- Consider seeing a pulmonologist specializing in complex breathing disorders
Remember: A true asthma diagnosis should bring relief—both in symptoms and in having answers. If your current treatment isn’t working, the problem might not be you—it might be the diagnosis itself.
Still Have Questions? We Have Answers.
Lung health is complex. If you’re wondering “What about…?” or “What’s next for me?”, you’re not alone. Our Resource Hub is built to be your **first stop for trustworthy, in-depth answers** on every aspect of respiratory wellness.
- Condition-Specific Guides (COPD, Asthma, Post-COVID)
- Step-by-Step Detox & Recovery Plans
- Science-Backed Natural & Conventional Strategies