Reclaim Your Sleep: A Practical Guide to Conquering Nighttime Bathroom Trips
Waking up once, twice, or even more each night with an urgent need to urinate—this is nocturia, and for men with BPH, it’s often the symptom that shatters sleep and drains energy. You’re not just losing rest; you’re losing quality of life.
The good news: Nocturia is manageable. While an enlarged prostate is often the root cause, the triggers are frequently within your control. This guide moves beyond generic advice to deliver BPH-specific nocturia fixes—actionable strategies that combine smart habits, positional changes, and targeted treatments to help you reduce those disruptive nighttime trips and enjoy uninterrupted sleep again.
Understanding “Why”: The BPH-Nocturia Connection
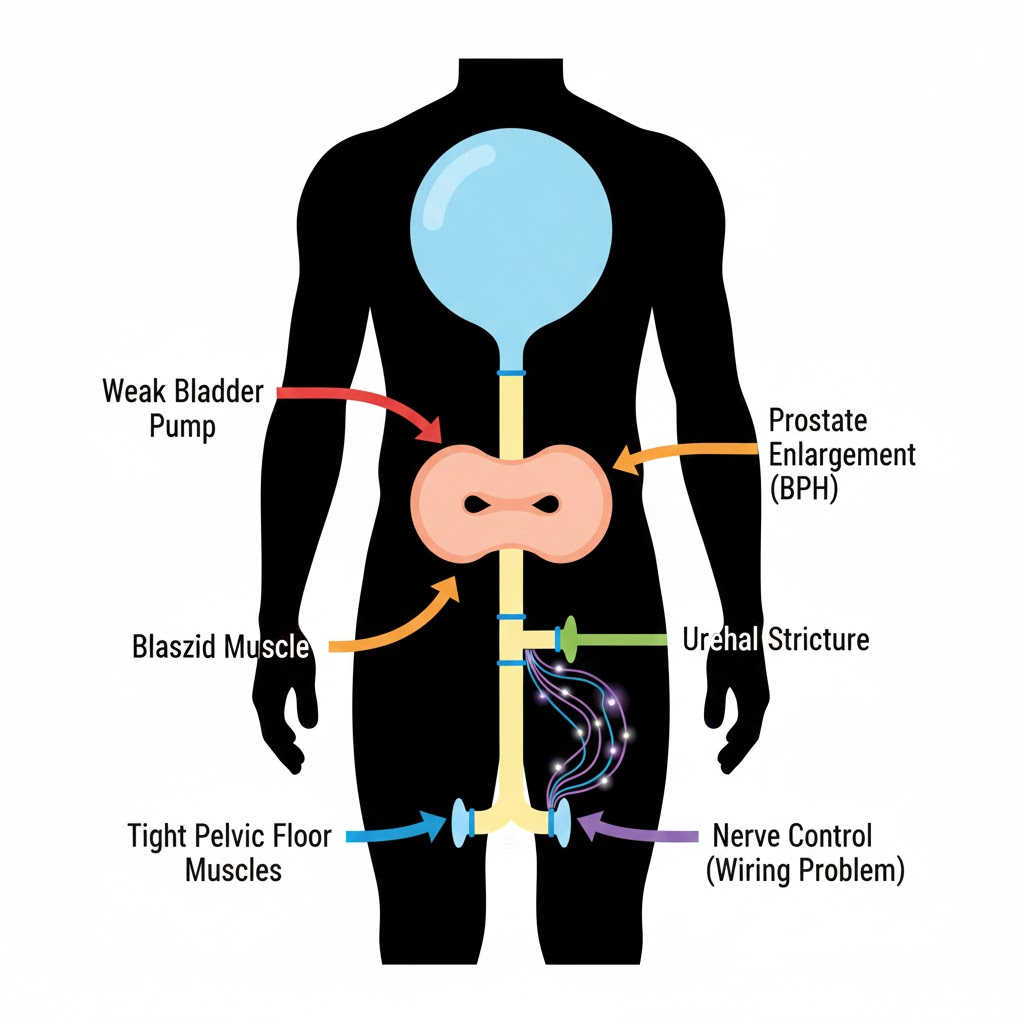
To fix nocturia, it helps to understand the mechanics. With BPH, two main issues conspire to ruin your night:
- Obstructed Storage: The enlarged prostate squeezes the urethra, making it harder for your bladder to empty completely during the day. This means it refills to capacity faster at night.
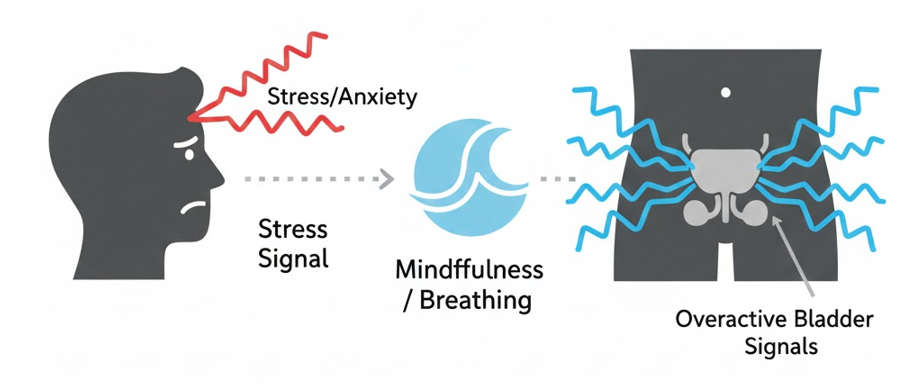
- Bladder Irritability: The constant struggle to push urine past the obstruction can make the bladder muscle (detrusor) overactive and hypersensitive, sending “FULL!” signals even when it’s not.
Additionally, as we age, the body’s natural rhythm of urine production changes. Younger bodies produce less urine at night; older bodies often lose this rhythm, leading to nocturnal polyuria—simply producing too much urine overnight.
Your strategy must address both the mechanical obstruction (through treatment) and the behavioral/physiological triggers.
Phase 1: Lifestyle & Behavioral Modifications (Your First Line of Defense)
These are the changes you can implement tonight. Consistency is key.
1. Master Fluid Management: It’s About When, Not Just How Much
- The 2-Hour Rule: Stop drinking all fluids 2-3 hours before bedtime. This includes water, tea, and especially alcohol.
- Front-Load Your Day: Ensure you’re drinking adequate fluids (about 3.7L for men) earlier in the day, finishing your major intake by early evening.
- Identify & Eliminate Diuretics: Caffeine (coffee, tea, soda) and alcohol are potent diuretics that increase urine production. Avoid them completely after mid-afternoon. Learn more in our guide on Caffeine, Alcohol, and BPH.
2. Optimize Sleep Position & Environment
- Elevate Your Legs: If you have mild swelling in your legs (edema), fluid can re-enter your bloodstream when you lie down, turning into urine. Prop your legs up on a pillow for 1-2 hours before bed to allow this fluid to process before sleep.
- Sleep on Your Side: Specifically, try sleeping in a fetal position. This can prevent the prostate from settling directly onto the bladder, reducing direct pressure and the sensation of fullness. Our dedicated article on Best Sleep Positions for BPH dives deeper.
- Create a Sleep-Safe Path: Use dim, motion-activated night lights to guide you to the bathroom. This minimizes full wakefulness, making it easier to fall back asleep.
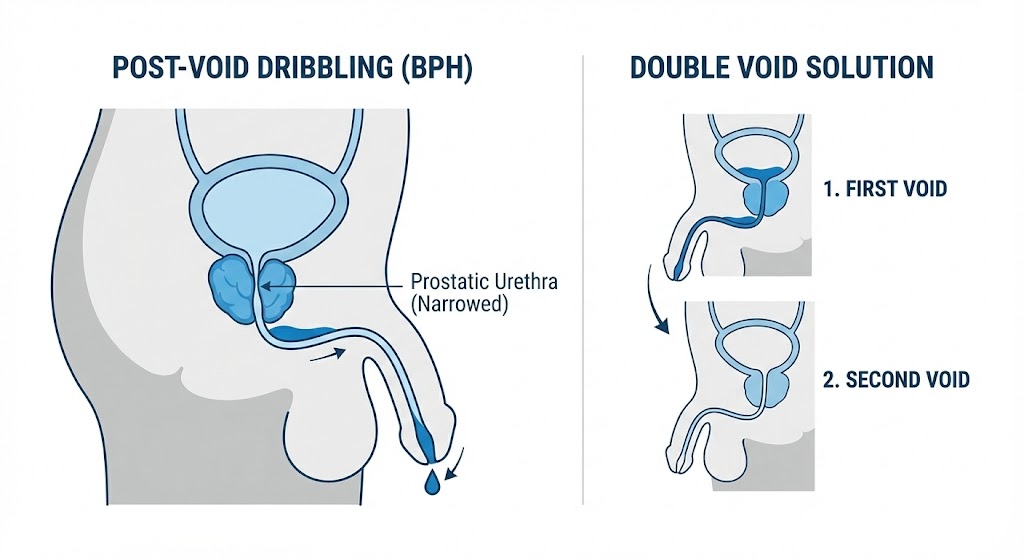
3. Practice Strategic “Double Voiding”
Right before you get into bed:
- Urinate as you normally would.
- Wait 30 seconds. Relax, shift your weight.
- Try to urinate again.
This technique helps empty the bladder more completely, buying you precious extra time.
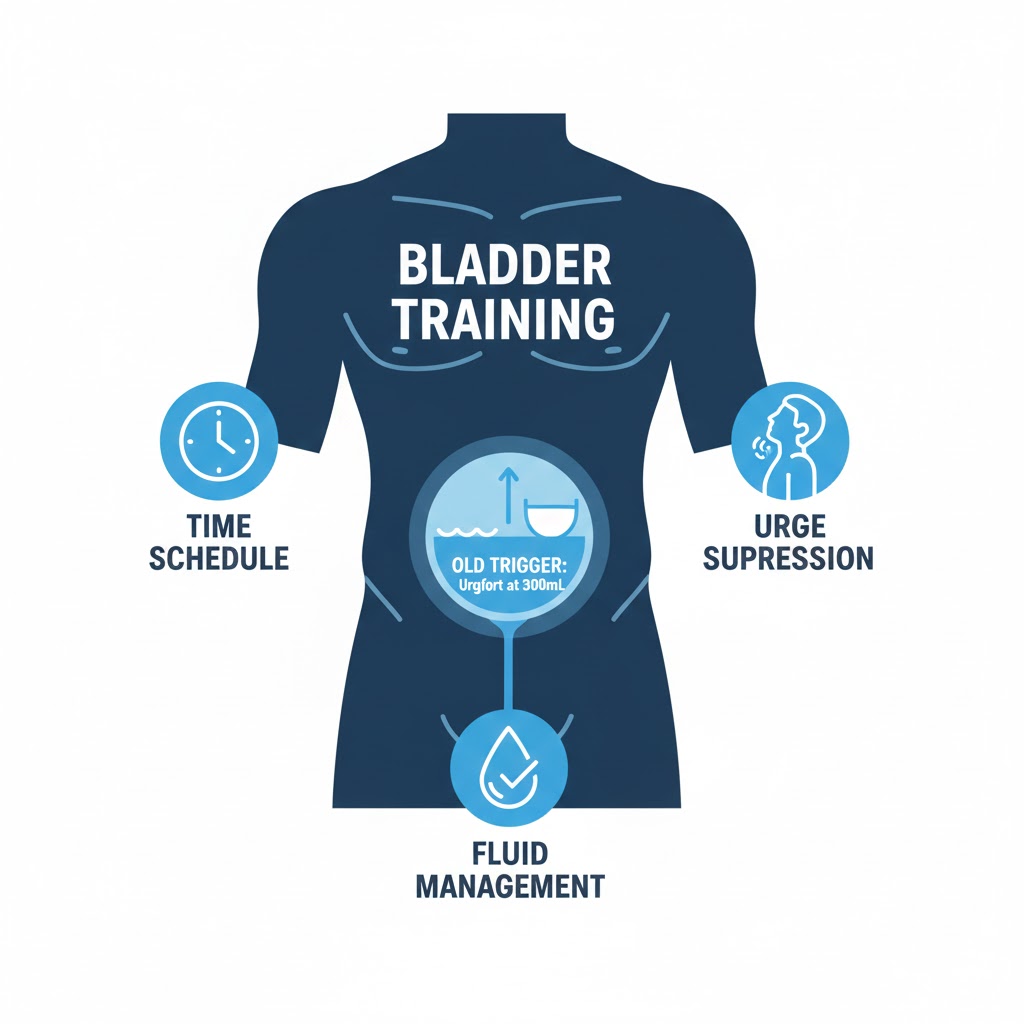
Phase 2: Bladder Retraining & Pelvic Floor Power
If urgency is a major component of your nocturia, these techniques are essential.
- Bladder Retraining: This behavioral therapy aims to increase the time between daytime urges, which in turn increases your functional bladder capacity at night. It involves consciously delaying urination by a few minutes when you feel an urge, gradually extending the interval. For a structured program, see our Bladder Retraining Guide for BPH.
- Pelvic Floor Exercises (Kegels for Men): A strong pelvic floor provides better support for your bladder and prostate and improves your ability to “hold it.” Crucially, it also helps with complete emptying, reducing residual urine. Learn the correct technique in our Step-by-Step Pelvic Floor Exercise Guide.
Phase 3: Medical Evaluation & Targeted Treatments
When lifestyle changes aren’t enough, it’s time to consult your doctor. Nocturia can also be a sign of other conditions like sleep apnea, uncontrolled diabetes, or heart failure.
Medications That Can Help:
- Desmopressin: A synthetic hormone that specifically reduces the amount of urine your kidneys produce at night. It’s a direct treatment for nocturnal polyuria.
- Anticholinergics or Beta-3 Agonists (e.g., Myrbetriq): Calm an overactive bladder muscle, reducing the urgency signals that wake you up.
- Your Standard BPH Medications: Alpha-blockers (Flomax) improve emptying, while 5-ARIs (Proscar, Avodart) slowly shrink the prostate. Both can indirectly improve nocturia over time.
Procedures to Address the Root Cause:
If nocturia is severe and linked to significant obstruction, treating the BPH itself may be the ultimate solution. Minimally invasive procedures like UroLift or Rezūm, or surgeries like TURP, can dramatically improve bladder emptying and reduce nighttime symptoms.
Your Action Plan: Start Tonight
- Track It: For 3 nights, log what time you drink, what you drink, and what time you wake up to urinate. Patterns will emerge.
- Implement One Change: Start with fluid curfew. Stop all drinks 2.5 hours before bed.
- Add a Second Tactic: The following week, add leg elevation for an hour before bed.
- Evaluate: After 2 weeks, has the frequency changed? If yes, continue. If no, move to bladder retraining during the day and consider a doctor’s visit to rule out other causes and discuss medications.
Conclusion
Nocturia doesn’t have to be a life sentence of broken sleep. By systematically addressing fluid intake, sleep mechanics, bladder function, and the underlying BPH, you can significantly reduce—and often nearly eliminate—nighttime trips. Start with the behavioral fixes you control, and partner with your urologist to explore medical solutions for lasting relief. Your path to uninterrupted sleep starts tonight.
FAQs
1. How many nighttime bathroom trips is considered “nocturia”?
Waking up once per night is generally considered normal, especially as you age. Nocturia is clinically defined as waking up two or more times per night to urinate. If it’s bothering you or affecting your daytime energy, it’s worth addressing.
2. Is it bad to just hold it until morning?
If you wake with a strong urge, it’s usually better to get up and empty your bladder. Regularly “holding it” against a strong urge can overstretch the bladder muscle, potentially worsening overactivity or leading to incomplete emptying, which can increase the risk of UTIs.
3. I only drink water. Why do I still have nocturia?
Even water contributes to urine volume. The issue is often timing. Drinking a large glass of water right before bed will result in urine production a few hours later. Also, BPH itself—causing incomplete emptying and bladder irritation—is the primary driver, not just fluid type.
4. Can a CPAP machine help with nocturia if I have sleep apnea?
Absolutely. Sleep apnea causes stress hormones to be released, which can increase urine production. Treating sleep apnea with a CPAP machine is one of the most effective ways to reduce nocturia in men who have both conditions. It’s a critical connection to check with your doctor.
5. Are there any specific bedtime snacks that help or hurt?
Avoid salty snacks before bed, as salt can make you thirsty and lead to increased fluid intake. Also, avoid high-sugar foods, which can have a mild diuretic effect. A small, bland snack like a few crackers is fine if you’re hungry.
6. Does exercising in the evening make nocturia worse?
It can, especially if you rehydrate heavily after a late workout. Try to finish intense exercise and your post-workout hydration at least 3 hours before bedtime. Gentle stretching or yoga in the evening is usually fine.
7. How does “double voiding” actually help?
When you urinate with BPH, the bladder may not contract fully due to the obstruction. Waiting a moment allows the detrusor muscle to reset and contract again, often releasing a surprising additional amount of urine. This leaves less in the tank to wake you up later.
8. When should I see a doctor specifically for nocturia?
See your doctor if: a) You’re waking up 3 or more times per night, b) Lifestyle changes for 2-3 weeks show no improvement, c) You experience pain, burning, or see blood in your urine, or d) You’re excessively thirsty, which could indicate diabetes.
9. Can certain medications cause nocturia?
Yes. Diuretics (“water pills” for blood pressure), some antidepressants, and even certain over-the-counter sleep aids or pain medications can increase urine production or affect bladder function. Never stop prescribed medication, but do review your full medication list with your doctor.
10. Will treating my BPH with medication or surgery cure my nocturia?
It often significantly improves it, but not always 100%. Procedures that improve bladder emptying (like TURP or UroLift) can have a dramatic effect. Medications like alpha-blockers can help. The goal is to reduce the frequency to 0-1 times per night, which is considered a successful treatment outcome.
Related Articles
- Sleep Positions for BPH: Reduce Bladder Pressure Overnight: Pair the strategies here with optimal sleeping posture.
- Bladder Retraining for BPH: Increase Your Capacity: A step-by-step program to lengthen the time between urges day and night.
- BPH Medications Guide: Alpha-Blockers vs. 5-ARIs: Understand how prescription drugs can help manage the root cause of nocturia.
- The Role of Stress Management in BPH Flare-Ups: Anxiety and stress can worsen urgency and frequency, including at night.
Looking for the Full Picture?
This is one chapter in our ultimate guide to prostate health.
Dive deeper into every aspect of BPH with our central resource hub, featuring over 30 detailed articles organized for your journey.
Visit the Main Hub: The Complete Guide to BPH & Prostate Health