Untangling the Two Most Common Prostate Problems
If you’re experiencing urinary discomfort, pain, or changes in flow, you’ve likely come across two terms: BPH (Benign Prostatic Hyperplasia) and prostatitis. While both affect the prostate and share some overlapping symptoms, they are fundamentally different conditions with distinct causes and treatments. Misunderstanding which you have can lead to months of frustration and ineffective remedies.
This guide provides a clear, side-by-side comparison to help you distinguish between an enlarged prostate (BPH) and prostate inflammation/infection (prostatitis), empowering you to have a more informed conversation with your urologist and pursue the correct treatment path from the start.
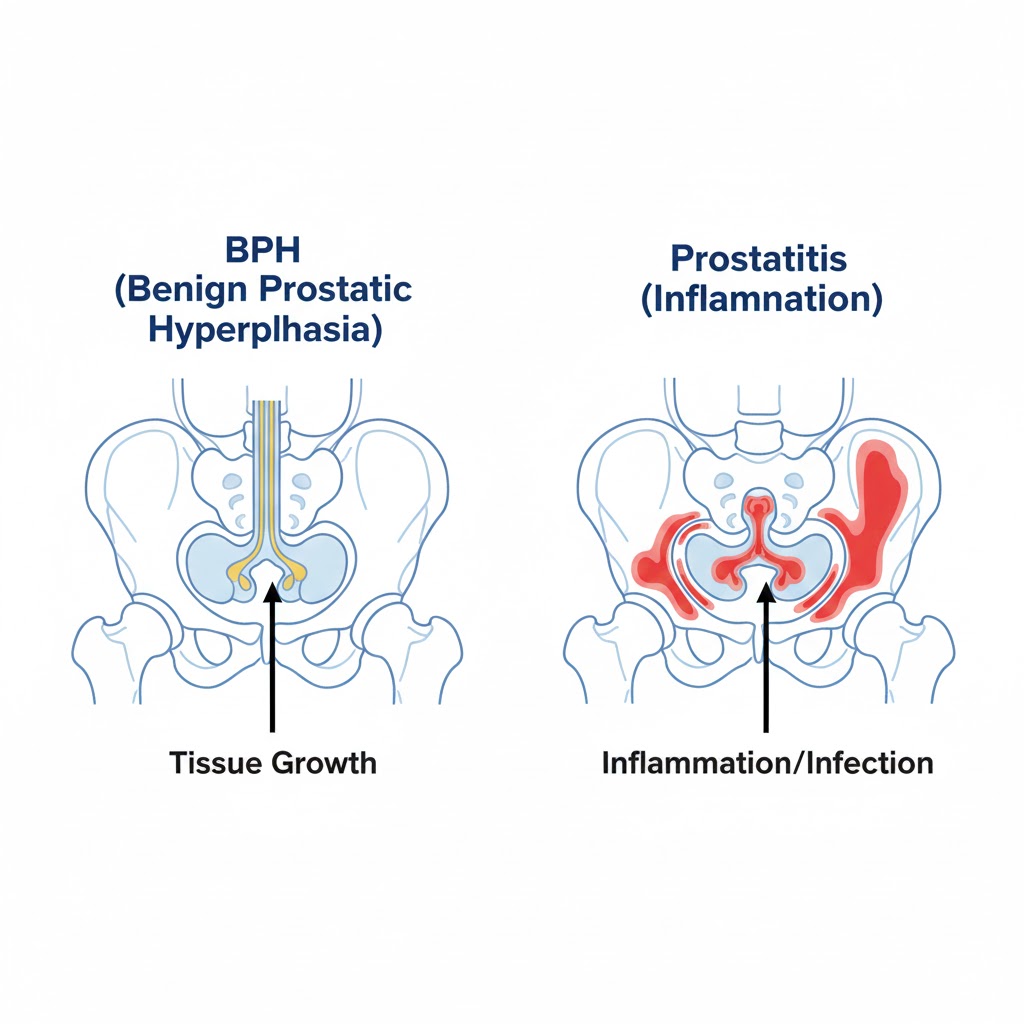
The Core Difference: Growth vs. Inflammation
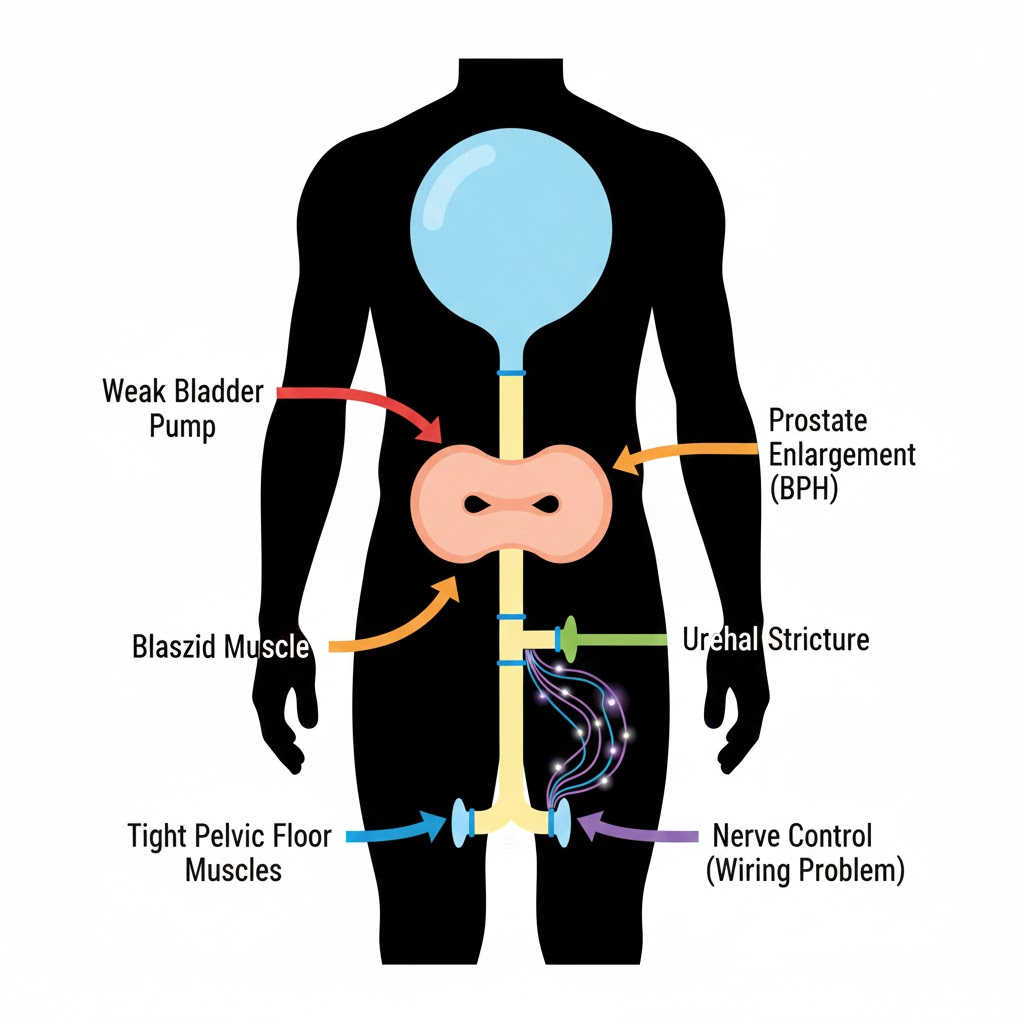
- BPH (Benign Prostatic Hyperplasia): This is a non-cancerous growth or enlargement of the prostate gland. It’s a mechanical and hormonal issue—the prostate physically gets larger and squeezes the urethra.
- Prostatitis: This refers to inflammation of the prostate gland. It can be caused by a bacterial infection (acute or chronic) or occur without a clear infectious cause (chronic pelvic pain syndrome). It’s primarily an inflammatory or infectious issue.
Think of it this way: BPH is like a slowly expanding sponge squeezing a water hose. Prostatitis is like that same hose being irritated, swollen, and painful from a chemical or infection.
Symptom Comparison: Where They Overlap and Diverge
This table highlights the key symptomatic differences, which are your first clues to distinguishing the conditions.
| Symptom | BPH (Enlarged Prostate) | Prostatitis (Prostate Inflammation) |
|---|---|---|
| Urinary Frequency | Common, especially nocturia (nighttime). | Common, often with urgent, painful need to go. |
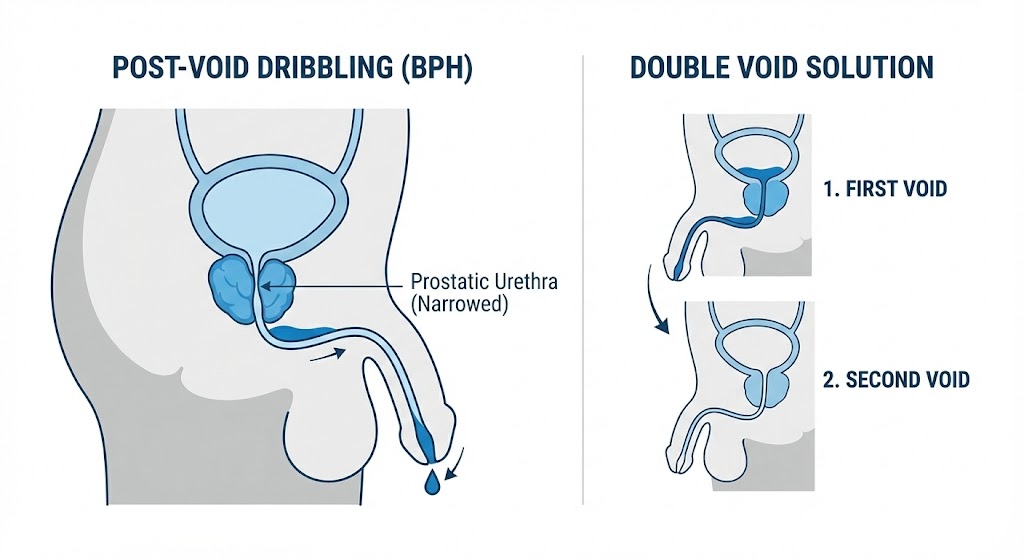
| Weak/Interrupted Stream | Hallmark symptom. Hesitancy, straining, dribbling. | May occur, but not usually the primary complaint. |
| Pain or Discomfort | Rare. May feel “pressure” but not sharp pain. | Hallmark symptom. Pain in pelvis, perineum (between scrotum and anus), lower back, or during/after ejaculation. |
| Burning with Urination | Uncommon. | Very common, especially with bacterial prostatitis. |
| Fever & Chills | No. | Yes, with acute bacterial prostatitis (a medical emergency). |
| Sexual Function | Can cause erectile issues; retrograde ejaculation is common post-treatment. | Often causes painful ejaculation, which can lead to avoidance of sex. |
| PSA Level | Often mildly to moderately elevated (scales with size). | Can be very highly elevated (even >10 ng/mL), usually drops after treatment. |
| Onset | Very gradual, over years. | Can be sudden and severe (acute) or come and go (chronic). |
The Pain Factor is Key: The single biggest differentiator is pain. If you have significant pain in your pelvis, genitals, or during urination/ejaculation, prostatitis is the much more likely culprit.
Causes and Risk Factors: Understanding the Roots
BPH Causes:
- Aging & Hormones: The primary drivers. As men age, testosterone converts to DHT, stimulating prostate cell growth.
- Family History: Genetics play a strong role.
- Metabolic Health: Obesity, diabetes, and heart disease are linked to more severe BPH.
Prostatitis Causes:
- Bacterial Infection: Bacteria from urine travel back into the prostate ducts. Can be acute (sudden, severe) or chronic (recurring).
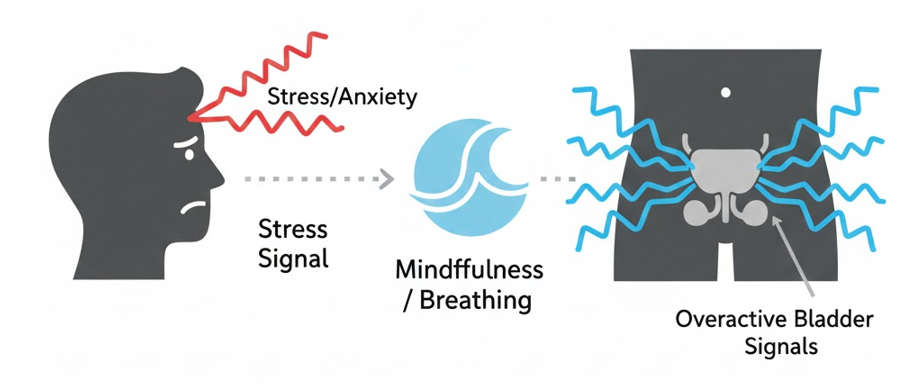
- Nerve/Muscle Dysfunction: In Chronic Pelvic Pain Syndrome (CPPS)—the most common type—the cause is often neuromuscular, involving pelvic floor muscle spasms.
- Autoimmune Response: The body’s immune system may mistakenly attack the prostate.
- Urinary Reflux: Urine flows backward into prostatic ducts, causing chemical irritation.
Diagnosis: How Doctors Tell Them Apart
Your urologist won’t rely on symptoms alone. Here’s what to expect:
- Medical History: They will ask detailed questions about pain location, sexual function, and symptom onset.
- Digital Rectal Exam (DRE):
- BPH: Prostate feels smooth but symmetrically enlarged.
- Prostatitis: Prostate may feel swollen, tender, or warm to the touch. Massaging it during the exam may express fluid for culture.
- Urinalysis & Culture: Critical for prostatitis. Checks for white blood cells (infection) and bacteria. A post-prostatic massage urine sample is the gold standard for diagnosing bacterial prostatitis.
- PSA Test: An elevated PSA is common in both. However, a very high PSA that drops significantly after antibiotics strongly suggests prostatitis.
- Symptom Questionnaires: Different standardized forms are used (IPSS for BPH, NIH-CPSI for prostatitis).
Treatment Paths: Why Getting the Right Diagnosis is Crucial
Treating BPH as if it were prostatitis (or vice versa) will fail. Here’s how treatments differ:
BPH Treatments Focus on:
- Relaxing Muscles or Shrinking Tissue: Alpha-blockers (Flomax), 5-alpha reductase inhibitors (Finasteride).
- Reducing Obstruction: Surgical procedures like TURP or UroLift.
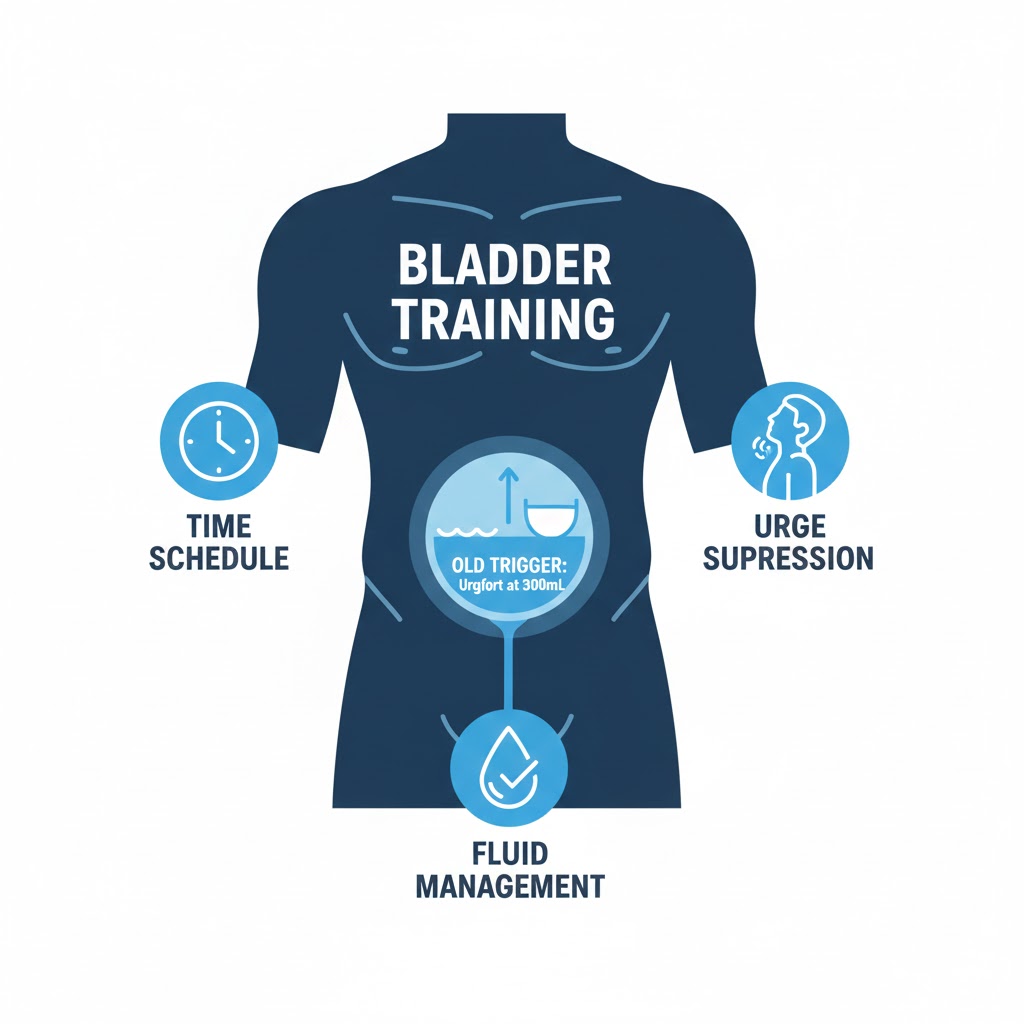
- Lifestyle Management: Diet, pelvic floor exercises, fluid timing.
Prostatitis Treatments Focus on:
- Eradicating Infection: Long-course antibiotics (4-6 weeks for chronic bacterial) are first-line for bacterial types.
- Reducing Inflammation & Pain: Alpha-blockers (to relax ducts), anti-inflammatories (NSAIDs), muscle relaxants.
- Physical Therapy: Pelvic floor physical therapy is a cornerstone treatment for CPPS to release muscle spasms.
- Stress & Pain Management: Biofeedback, relaxation techniques, neuromodulators (like gabapentin).
Can You Have Both Conditions?
Yes, it’s possible to have “Prostatitis/BPH Overlap Syndrome.” An existing, enlarged prostate (BPH) may be more prone to infection or inflammation (prostatitis). This can make diagnosis and treatment more complex, requiring a urologist to address both the mechanical obstruction and the inflammatory/infectious component.
Conclusion: The Path to the Right Diagnosis Starts Here
If you take away one thing, let it be this: Persistent pelvic or urinary pain warrants a prostatitis evaluation, while painless but progressive difficulties with urine flow point toward BPH.
Your Action Plan:
- Track Your Symptoms: Note specifically where it hurts and when (during urination? after sex?).
- Schedule a Urologist Visit: Be prepared to describe your symptoms in detail using the distinctions above.
- Ask for Specific Tests: Request a urinalysis with culture and discuss the possibility of prostatitis if pain is a factor.
- Consider Pelvic Floor Evaluation: If antibiotics don’t help chronic pain, ask about a referral to a pelvic floor physical therapist.
Understanding this fundamental difference is your first and most powerful step toward effective treatment and lasting relief.
Navigate Our Complete BPH Hub:
- Silo 1: BPH Symptoms & Daily Management (You are here)
- Silo 2: Medical & Surgical Treatments
- Silo 3: Natural Remedies & Lifestyle
- Main Hub: The Complete Guide to BPH & Prostate Health
FAQs
1. Can prostatitis cause an enlarged prostate (BPH)?
Prostatitis can cause the prostate to become swollen and feel enlarged during an acute flare-up due to inflammation and edema. However, this is temporary swelling, not the actual tissue growth that defines BPH. The two conditions are distinct, though they can co-exist.
2. Which condition causes a higher PSA level?
Acute bacterial prostatitis can cause PSA levels to spike dramatically, sometimes to very high levels (e.g., over 20 ng/mL). BPH typically causes a more gradual, moderate elevation that correlates with prostate size. After successful prostatitis treatment, PSA should drop significantly.
3. I have urinary frequency but no pain. Could it still be prostatitis?
Yes, particularly with non-bacterial chronic prostatitis/chronic pelvic pain syndrome (CPPS). The “pain” component can sometimes be perceived as discomfort, pressure, or unusual sensation rather than sharp pain. Frequency and urgency without obstruction can be hallmarks of the inflammatory types.
4. Can BPH medications like Flomax help prostatitis?
Sometimes, yes. Alpha-blockers (Flomax) are often prescribed for prostatitis/CPPS not because they shrink the prostate, but because they relax the smooth muscle in the prostate ducts and bladder neck, improving drainage and reducing pain. They treat a symptom, not the root cause of inflammation.
5. How long does prostatitis last compared to BPH?
BPH is a chronic, lifelong condition that progresses slowly. Prostatitis can be: Acute (sudden, severe, resolves with antibiotics in weeks), Chronic Bacterial (recurring infections over months/years), or Chronic Pelvic Pain Syndrome (CPPS) (pain lasting >3 months, often without infection). CPPS can be a long-term management issue.
6. Does ejaculation help or hurt with each condition?
- BPH: Regular ejaculation is generally neutral or possibly beneficial, as it may help relieve ductal congestion.
- Prostatitis: This is highly individual. For some, ejaculation can worsen pain (especially immediately after). For others, it may provide temporary relief. Painful ejaculation is a red flag for prostatitis.
7. Can stress cause prostatitis or BPH?
- BPH: Stress doesn’t cause it, but can worsen symptoms (urgency, frequency).
- Prostatitis/CPPS: Stress is considered a major trigger and exacerbating factor for flare-ups, likely through muscle tension and nervous system effects. Stress management is a key part of treatment.
8. Which condition is more common in younger men (under 50)?
Prostatitis/CPPS is far more common in younger men (20s-40s). BPH is primarily an age-related condition, though early signs can appear in the 40s and 50s. A young man with urinary symptoms and pain should first be evaluated for prostatitis.
9. Do both conditions increase prostate cancer risk?
No. Neither BPH nor prostatitis is known to cause or increase the risk of prostate cancer. They involve different biological processes. However, both can elevate PSA, which complicates cancer screening.
10. What’s the first test a doctor should do to tell them apart?
A urinalysis with culture is the critical first test. The presence of white blood cells and/or bacteria strongly points toward prostatitis (especially bacterial). If the urine is clean and symptoms are obstructive without pain, BPH becomes the leading suspect.
Related Articles
- PSA Test: What Your Results Really Mean: Understand why PSA can spike with prostatitis and how it’s interpreted differently than in BPH.
- BPH Self-Assessment Quiz & Symptom Tracker: Use the IPSS form to quantify your obstructive symptoms.
- Pelvic Floor Exercises for BPH & Prostatitis: Learn how physical therapy can help both conditions through different mechanisms.
- The Role of Stress Management in Reducing Flare-Ups: Essential reading for managing prostatitis/CPPS symptoms.
Considering a Natural Prostate Supplement?
Many of our readers have asked about comprehensive natural formulas. Prostavive combines 9 research-backed ingredients including Saw Palmetto, Beta-Sitosterol, and Pygeum in one supplement.
Note: This is an affiliate link. We earn a commission if you purchase, at no extra cost to you. Always consult your healthcare provider before starting supplements.
Looking for the Full Picture?
This is one chapter in our ultimate guide to prostate health.
Dive deeper into every aspect of BPH with our central resource hub, featuring over 30 detailed articles organized for your journey.
Visit the Main Hub: The Complete Guide to BPH & Prostate Health