Understanding why the immune system targets the thyroid — and what women can do naturally
Autoimmune thyroid conditions are the leading cause of thyroid dysfunction in women.
Yet many women are diagnosed with “thyroid problems” without ever being told their immune system may be the real driver.
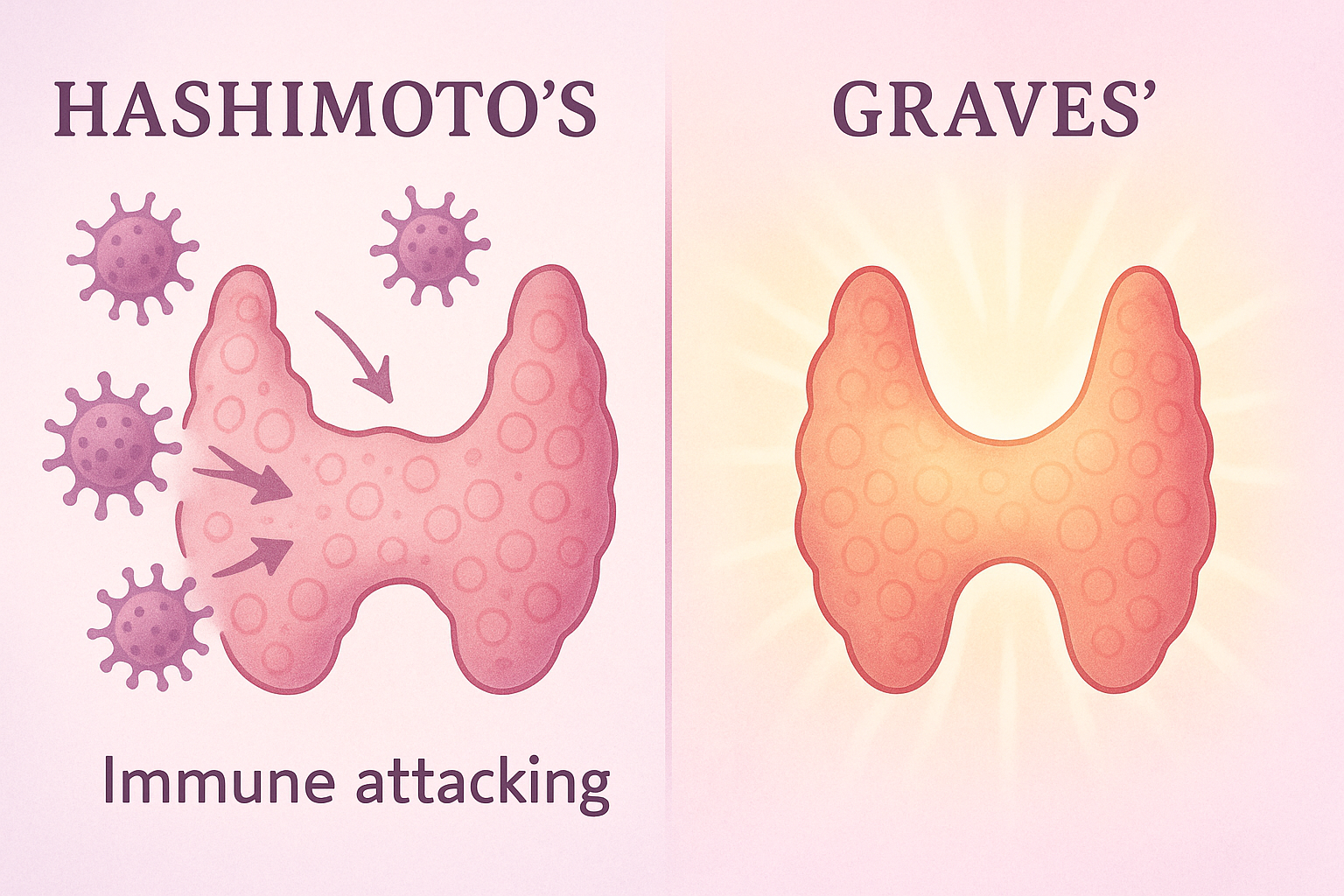
Two autoimmune diseases dominate thyroid-related diagnoses:
- Hashimoto’s Thyroiditis (most common cause of hypothyroidism)
- Graves’ Disease (most common cause of hyperthyroidism)
Understanding how autoimmunity affects the thyroid is critical — because treating hormone levels alone often misses the root cause.
This guide explains how autoimmune conditions impact thyroid health, the key differences between Hashimoto’s and Graves’, common triggers, symptoms, testing, and natural support strategies for women.
🔍 What Is an Autoimmune Thyroid Condition?
An autoimmune condition occurs when the immune system mistakenly attacks healthy tissue.
In autoimmune thyroid disease, the immune system targets thyroid cells or thyroid-related enzymes, leading to inflammation and dysfunction.
Instead of regulating hormones, the immune system:
- Produces antibodies
- Triggers chronic inflammation
- Gradually damages thyroid tissue
Over time, this disrupts the production of thyroid hormones (T3 and T4).
➡ Related reading:
The Connection Between Thyroid Hormones, T3 and T4
🧠 The Two Main Autoimmune Thyroid Conditions
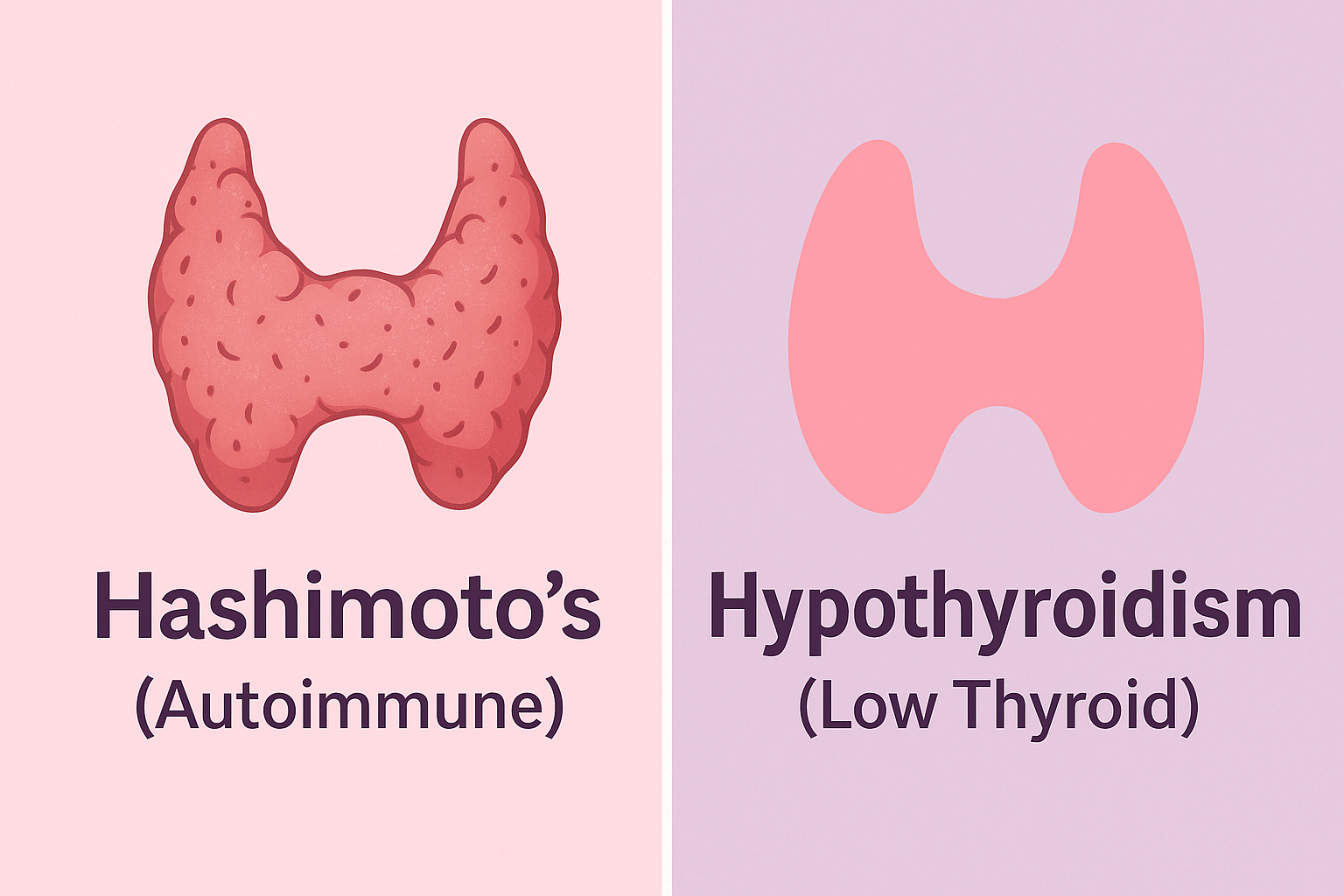
🔥 Hashimoto’s Thyroiditis (Autoimmune Hypothyroidism)
Hashimoto’s causes the immune system to slowly destroy the thyroid gland, resulting in low thyroid hormone levels.
Common features:
- Elevated thyroid antibodies (TPOAb, TGAb)
- Gradual onset of hypothyroidism
- Fluctuating symptoms in early stages
- Strong link to stress, pregnancy, menopause, and estrogen dominance
➡ Deep dive:
The Difference Between Hashimoto’s and Hypothyroidism in Women
⚡ Graves’ Disease (Autoimmune Hyperthyroidism)
Graves’ disease occurs when antibodies stimulate the thyroid, forcing it to produce too much hormone.
Common features:
- Elevated thyroid-stimulating immunoglobulins (TSI)
- Symptoms of hyperthyroidism
- Faster onset than Hashimoto’s
- Often triggered by acute stress or hormonal shifts
➡ Related article:
Signs of an Overactive Thyroid (Hyperthyroidism) in Women
⚖️ Hashimoto’s vs Graves’: Key Differences
| Feature | Hashimoto’s | Graves’ |
|---|---|---|
| Immune action | Destroys thyroid tissue | Overstimulates thyroid |
| Hormone levels | Low (hypothyroid) | High (hyperthyroid) |
| Speed of onset | Slow, progressive | Faster, more dramatic |
| Antibodies | TPOAb, TGAb | TSI |
| Common in women | Yes | Yes |
| Can fluctuate | Yes | Less commonly |
🚨 Common Symptoms of Autoimmune Thyroid Disease
Shared symptoms (autoimmune-related):
- Chronic fatigue
- Brain fog
- Joint pain
- Inflammation
- Sensitivity to stress
- Mood changes or anxiety
➡ Related:
The Link Between Thyroid and Mood Swings or Anxiety
Hashimoto’s-dominant symptoms:
- Weight gain
- Cold intolerance
- Dry skin
- Hair thinning
- Constipation
➡ See:
Signs of an Underactive Thyroid in Women
Graves’-dominant symptoms:
- Rapid heartbeat
- Weight loss
- Heat intolerance
- Tremors
- Anxiety
- Sleep disruption
🧪 How Autoimmune Thyroid Disease Is Diagnosed
Standard TSH tests are not enough.
A full thyroid + autoimmune panel should include:
- TSH
- Free T3
- Free T4
- Thyroid Peroxidase Antibodies (TPOAb)
- Thyroglobulin Antibodies (TGAb)
- Thyroid-Stimulating Immunoglobulins (TSI)
Without antibody testing, autoimmune thyroid disease is frequently missed or misclassified.
🧬 Why Women Are More Affected
Women are 5–10x more likely to develop autoimmune thyroid disease due to:
- Estrogen–immune system interaction
- Pregnancy and postpartum immune rebound
- Perimenopause and menopause hormone shifts
- Chronic stress and cortisol dysregulation
➡ Related reading:
The Connection Between Estrogen Dominance and Thyroid Issues
Postpartum Thyroid Changes: What Every Woman Should Know
🌿 Natural Strategies to Support Autoimmune Thyroid Health
1️⃣ Reduce Immune Triggers
- Identify food sensitivities (gluten, dairy)
- Support gut health
- Address chronic infections
➡ Related:
Foods That Harm Thyroid Health (and What to Avoid)
2️⃣ Balance Stress and Cortisol
Chronic stress worsens autoimmune activity and suppresses thyroid conversion.
➡ See:
How Stress Impacts Your Thyroid
Balancing Thyroid and Adrenal Fatigue Naturally
3️⃣ Optimize Key Nutrients
- Selenium (immune modulation)
- Zinc
- Magnesium
- Iron (if deficient)
- Vitamin D
➡ Related:
10 Essential Vitamins and Minerals for a Healthy Thyroid
4️⃣ Consider Targeted Thyroid Support
Women with autoimmune thyroid disease often benefit from nutrient-based support alongside lifestyle changes.
➡ Learn how to choose safely:
How to Choose the Right Thyroid Supplement for You
🩷 Final Thoughts
Autoimmune thyroid disease is not just a hormone problem — it’s an immune system imbalance.
Understanding whether Hashimoto’s or Graves’ is driving your symptoms allows you to:
- Seek proper testing
- Reduce inflammation
- Support your thyroid more effectively
- Avoid years of trial-and-error treatment
With the right information and holistic approach, many women see meaningful improvements in energy, mood, and quality of life.
❓ Frequently Asked Questions
1. What causes autoimmune thyroid disease?
Autoimmune thyroid disease occurs when the immune system mistakenly attacks the thyroid gland. Common triggers include chronic stress, hormonal changes (pregnancy, menopause), nutrient deficiencies, gut health imbalances, infections, and genetic susceptibility.
2. Is Hashimoto’s more common than Graves’ disease?
Yes. Hashimoto’s thyroiditis is significantly more common than Graves’ disease and is the leading cause of hypothyroidism in women. Graves’ disease is less common and primarily causes hyperthyroidism.
3. Can autoimmune thyroid disease go into remission?
In many women, yes. While autoimmune conditions are considered chronic, symptoms and antibody levels can often be reduced through stress management, dietary changes, gut support, and proper nutrient intake. Some women achieve long-term remission with a holistic approach.
4. Do thyroid medications treat autoimmunity?
No. Thyroid medications help regulate hormone levels but do not address the immune system dysfunction causing autoimmune thyroid disease. Supporting immune balance, reducing inflammation, and addressing triggers are essential alongside medication when needed.
5. Can stress trigger autoimmune thyroid disease?
Yes. Chronic stress elevates cortisol, which disrupts immune regulation and thyroid hormone conversion. Stress is a well-known trigger for both the onset and flare-ups of Hashimoto’s and Graves’ disease in women.
6. Is Graves’ disease reversible?
Graves’ disease can often be managed and put into remission, especially when identified early. Reducing immune stimulation, managing stress, correcting nutrient deficiencies, and working closely with a healthcare provider can significantly improve outcomes.
7. Are autoimmune thyroid conditions genetic?
There is a genetic component, meaning autoimmune thyroid disease can run in families. However, genetics alone do not cause the condition — environmental factors and lifestyle triggers play a major role in whether it develops.
8. Can pregnancy trigger thyroid autoimmunity?
Yes. Pregnancy and the postpartum period are common times for autoimmune thyroid conditions to appear or worsen due to immune system shifts. Postpartum thyroiditis is often autoimmune in nature and may evolve into Hashimoto’s.
9. Does diet matter for autoimmune thyroid disease?
Absolutely. Diet plays a major role in immune regulation and inflammation. Many women benefit from reducing inflammatory foods, supporting gut health, and ensuring adequate intake of key nutrients like selenium, zinc, and vitamin D.
10. Can supplements help autoimmune thyroid conditions?
Yes, when used appropriately. Supplements can help correct nutrient deficiencies, support immune balance, and reduce inflammation. However, they should complement — not replace — lifestyle changes and medical guidance, especially for autoimmune thyroid disease.
Looking for Targeted Thyroid Support?
If you’re dealing with low energy, stubborn weight changes, mood swings, or “thyroid fatigue” symptoms, a targeted thyroid-support formula may help fill common nutritional gaps and support healthy hormone balance.
- Designed for women: supports metabolism, energy, and daily thyroid function
- Convenient: easy daily routine alongside food-first habits
- Best used with: stress support, sleep improvements, and thyroid-friendly nutrition
Prefer to research first? Read the full breakdown here: Thyrafemme Review →
Note: This content is for informational purposes only and is not medical advice. Always consult a qualified healthcare professional before starting new supplements—especially if you are pregnant, breastfeeding, have a thyroid condition, or take thyroid medication.