If your knees ache when you stand…
If your fingers feel stiff in the morning…
If your hips, shoulders, or lower back hurt “out of nowhere”…
You are not imagining it.
Joint pain and inflammation are very common during perimenopause and menopause, even in women who never had joint problems before. The cause is not aging alone — it’s largely hormonal.
The good news is that with the right approach, joint pain during menopause can be significantly reduced — and often reversed.
This guide explains why menopause affects your joints and what actually works to restore comfort and mobility.
⭐ Why Menopause Causes Joint Pain and Inflammation
Menopausal joint pain is driven by a combination of hormonal decline, inflammation, and metabolic changes.
1️⃣ Estrogen Decline Increases Inflammation
Estrogen is a natural anti-inflammatory hormone.
As estrogen drops during menopause, inflammation rises throughout the body — including in joints and connective tissue.
This leads to:
- Achy joints
- Morning stiffness
- Swelling
- Reduced flexibility
Learn more here:
👉 What Really Happens to Your Hormones During Menopause
2️⃣ Cartilage Loses Protection
Estrogen helps maintain:
- Cartilage hydration
- Collagen integrity
- Joint lubrication
When estrogen declines:
- Cartilage thins
- Joints lose cushioning
- Friction and discomfort increase
This is why pain often appears suddenly during menopause.
3️⃣ Cortisol & Stress Worsen Joint Pain
Chronic stress increases cortisol, which:
- Raises inflammation
- Slows tissue repair
- Worsens pain sensitivity
Read more:
👉 How Stress and Cortisol Worsen Menopause Symptoms
4️⃣ Poor Sleep Increases Pain Sensitivity
Sleep disruption amplifies pain signals in the brain.
Night sweats and insomnia reduce the body’s ability to repair joints overnight.
👉 How to Sleep Better Through Menopause
5️⃣ Weight Changes Add Joint Stress
Menopause-related weight gain increases pressure on:
- Knees
- Hips
- Lower back
Even small increases can worsen joint pain.
👉 Menopause Weight Gain: Causes and Proven Solutions
🧠 Common Menopause-Related Joint Symptoms
- Knee pain
- Hip stiffness
- Shoulder discomfort
- Finger and wrist stiffness
- Lower back pain
- Morning stiffness
- Reduced range of motion
Many women describe feeling “older overnight” — but this is hormonal, not inevitable aging.
🌿 Proven Natural Ways to Reduce Joint Pain During Menopause
Below are science-backed strategies that address the root causes of menopause-related joint pain.
1️⃣ Reduce Inflammation with Food
An anti-inflammatory diet is one of the most powerful tools for joint relief.
Best foods for joint health:
- Fatty fish (salmon, sardines)
- Olive oil
- Berries
- Leafy greens
- Turmeric
- Ginger
- Nuts and seeds
Avoid:
- Refined sugar
- Processed foods
- Excess alcohol
👉 The Best Foods for Balancing Menopause Hormones
2️⃣ Gentle, Consistent Movement
Movement lubricates joints and reduces stiffness.
Best options:
- Walking
- Swimming
- Pilates
- Yoga
- Light strength training
Avoid long periods of sitting — even standing up every hour helps.
3️⃣ Support Bone & Joint Nutrients
Certain nutrients become especially important during menopause:
- Magnesium – reduces muscle tension & inflammation
- Vitamin D3 – supports bone and immune health
- Omega-3 fatty acids – powerful anti-inflammatory
- Collagen – supports cartilage and connective tissue
👉 Preventing Osteoporosis After Menopause
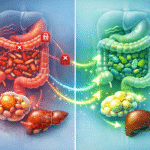
4️⃣ Improve Gut Health to Lower Inflammation
Inflammation often starts in the gut.
Supporting gut health helps:
- Reduce systemic inflammation
- Improve nutrient absorption
- Support immune balance
👉 The Role of Gut Health in Menopause
5️⃣ Manage Stress to Reduce Pain Signals
Lowering stress reduces inflammation and pain sensitivity.
Effective stress reducers:
- Deep breathing
- Gentle yoga
- Walking in nature
- Journaling
- Mindfulness practices
👉 Mindfulness and Meditation for Menopause Relief
6️⃣ Balance Hormones Naturally
Because estrogen decline is a major driver of joint pain, supporting hormonal balance often reduces symptoms significantly.
Natural menopause supplements that include:
- Red Clover
- Black Cohosh
- Magnesium
- Vitamin B6
- Anti-inflammatory herbs
can help calm systemic inflammation.
One doctor-developed option many women use is Menovelle.
👉 Order Menovelle (Official Page)
You’re Not Alone in This Transition
Menopause is not a single symptom — it’s a whole-body transition that deserves understanding and support.
Inside our Menopause Hub, you’ll find trusted, science-based articles covering:
- Hormones, hot flashes, sleep & weight changes
- Mood swings, anxiety, brain fog & confidence
- Nutrition, exercise & daily habits that help
- Natural menopause supplements & comparisons
❓ Frequently Asked Questions (FAQs)
1. Can menopause really cause joint pain?
Yes — estrogen decline directly increases inflammation and joint sensitivity.
2. Which joints are most affected?
Knees, hips, hands, shoulders, and lower back.
3. Does joint pain go away after menopause?
For many women, it improves once hormones stabilize.
4. Can supplements help joint pain?
Yes — especially magnesium, omega-3s, and hormone-supportive blends.
5. Is exercise safe with joint pain?
Yes — gentle, low-impact movement is highly beneficial.
6. Does weight gain worsen joint pain?
Yes — extra weight increases joint load and inflammation.
7. Does inflammation increase during menopause?
Yes — lower estrogen allows inflammation to rise.
8. Can stress make joint pain worse?
Absolutely — cortisol heightens pain sensitivity.
9. Should I use painkillers daily?
Occasional use is okay, but addressing root causes is safer long-term.
10. When should I see a doctor?
If pain is severe, swelling is persistent, or mobility is limited.