When It’s Not Just Your Prostate: Looking Beyond BPH for Urinary Flow Problems
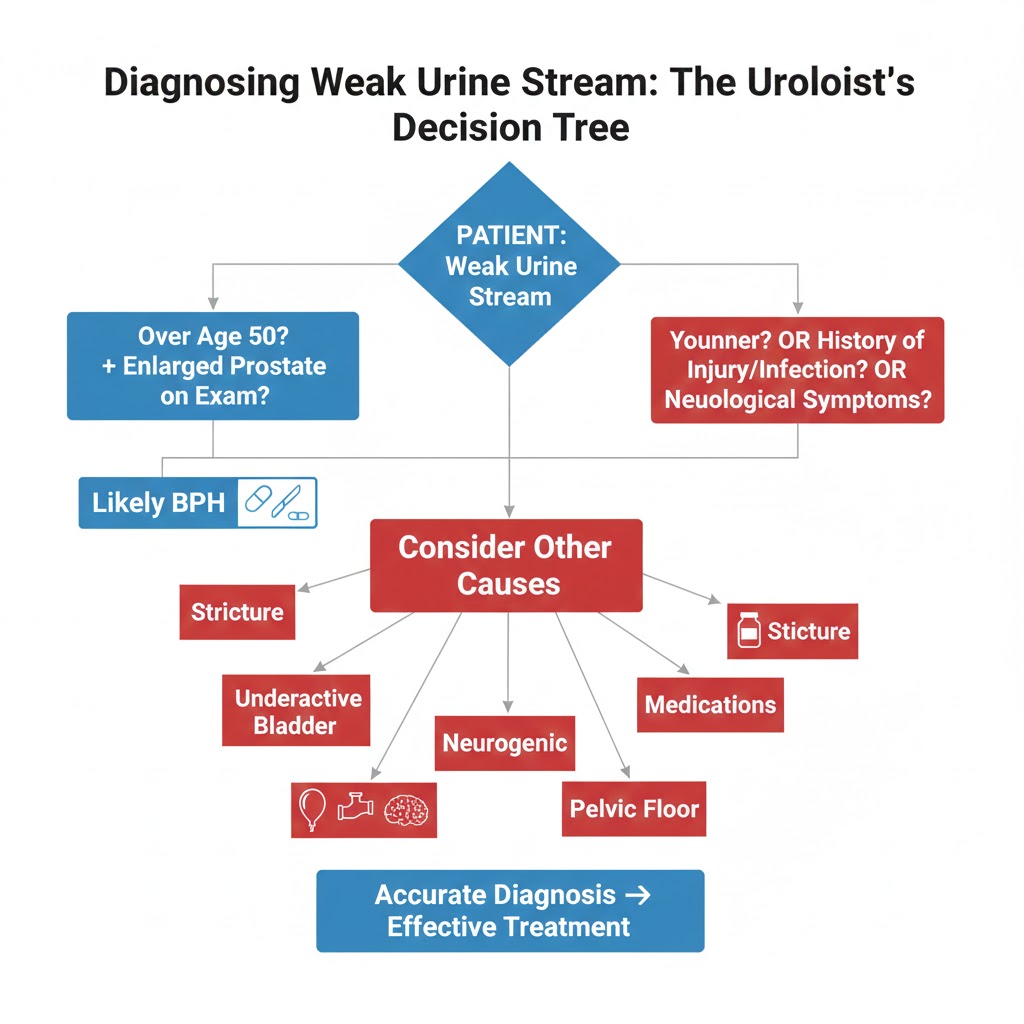
A weak, hesitant, or interrupted urine stream is often the first sign that sends men to the urologist, with BPH (enlarged prostate) being the immediate suspect. While BPH is indeed the most common cause in men over 50, it’s not the only possibility. Assuming it’s “just BPH” without proper evaluation can lead to ineffective treatment and prolonged discomfort.
This guide explores the other culprits behind a diminished urine stream. Understanding these alternative diagnoses empowers you to ask the right questions and ensures you receive the correct treatment, not just the most common one.
The Diagnostic Challenge: Why “Weak Stream” Needs Investigation
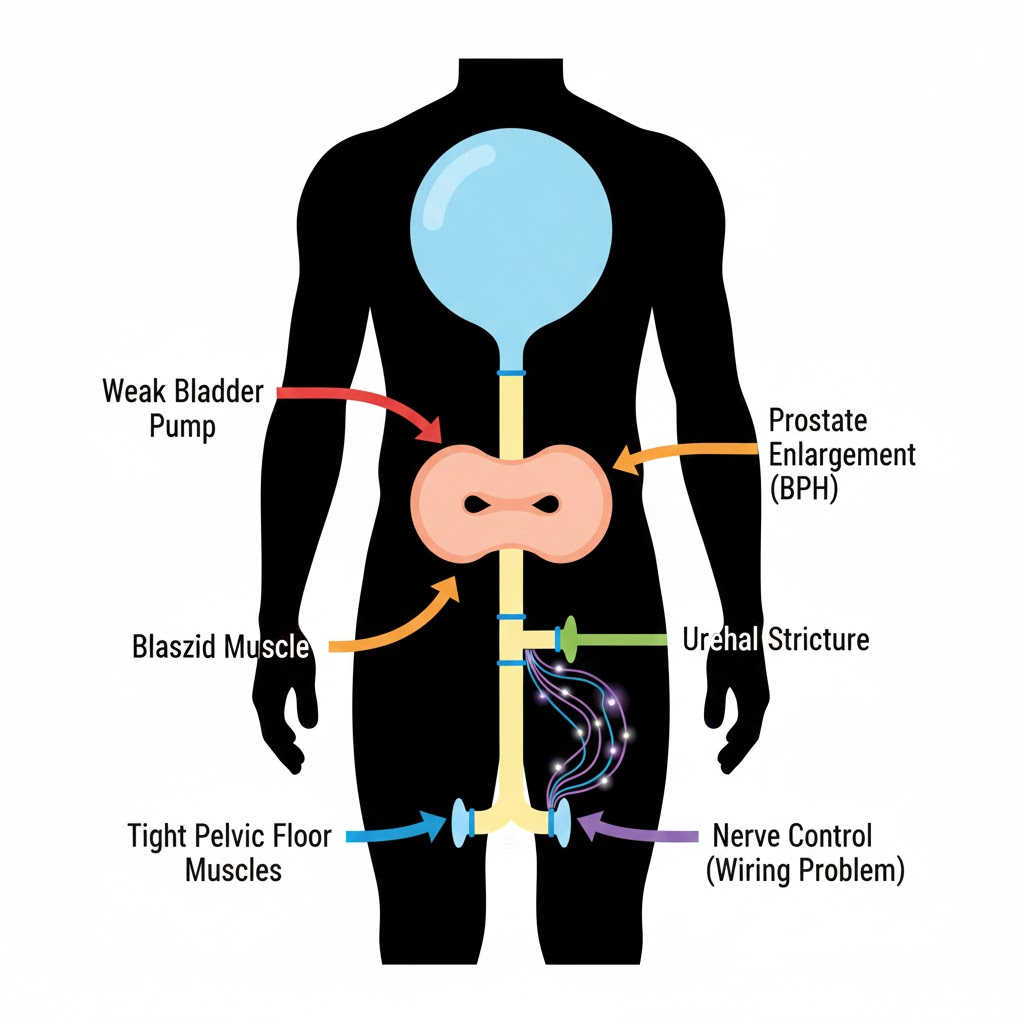
A weak stream is a symptom, not a diagnosis. It simply means something is obstructing or impairing the normal expulsion of urine from the bladder. That obstruction can occur at multiple points along the urinary tract:
- Bladder (the pump)
- Prostate (the valve and surround)
- Urethra (the pipe)
- Nervous System (the wiring)
A proper urological workup is designed to pinpoint the exact location and cause. Rushing to BPH treatment without this can be like fixing the ignition when the real problem is a flat tire.
The 5 Key Causes of Weak Urine Stream (That Aren’t BPH)
1. Urethral Stricture: The Scarred Pipe
- What it is: A narrowing of the urethra due to scar tissue formation.
- Common Causes: Previous urinary catheterizations, infections (especially STIs like gonorrhea), trauma, or instrumentation.
- How it Differs from BPH: Symptoms often start earlier in life (30s-40s). The stream may be forceful but very narrow (like a pencil). There may be a history of painful urination or infections preceding the flow change.
- Diagnosis: Urethroscopy (a camera into the urethra) or a retrograde urethrogram (X-ray with contrast).
- Treatment: Dilation, internal incision (urethrotomy), or surgical reconstruction.
2. Underactive Bladder (Detrusor Underactivity): The Weak Pump
- What it is: The bladder muscle (detrusor) fails to contract with enough force or duration to empty completely.
- Common Causes: Aging, diabetes (neuropathy), neurological conditions (Parkinson’s, MS, stroke), chronic over-distension from long-term untreated obstruction.
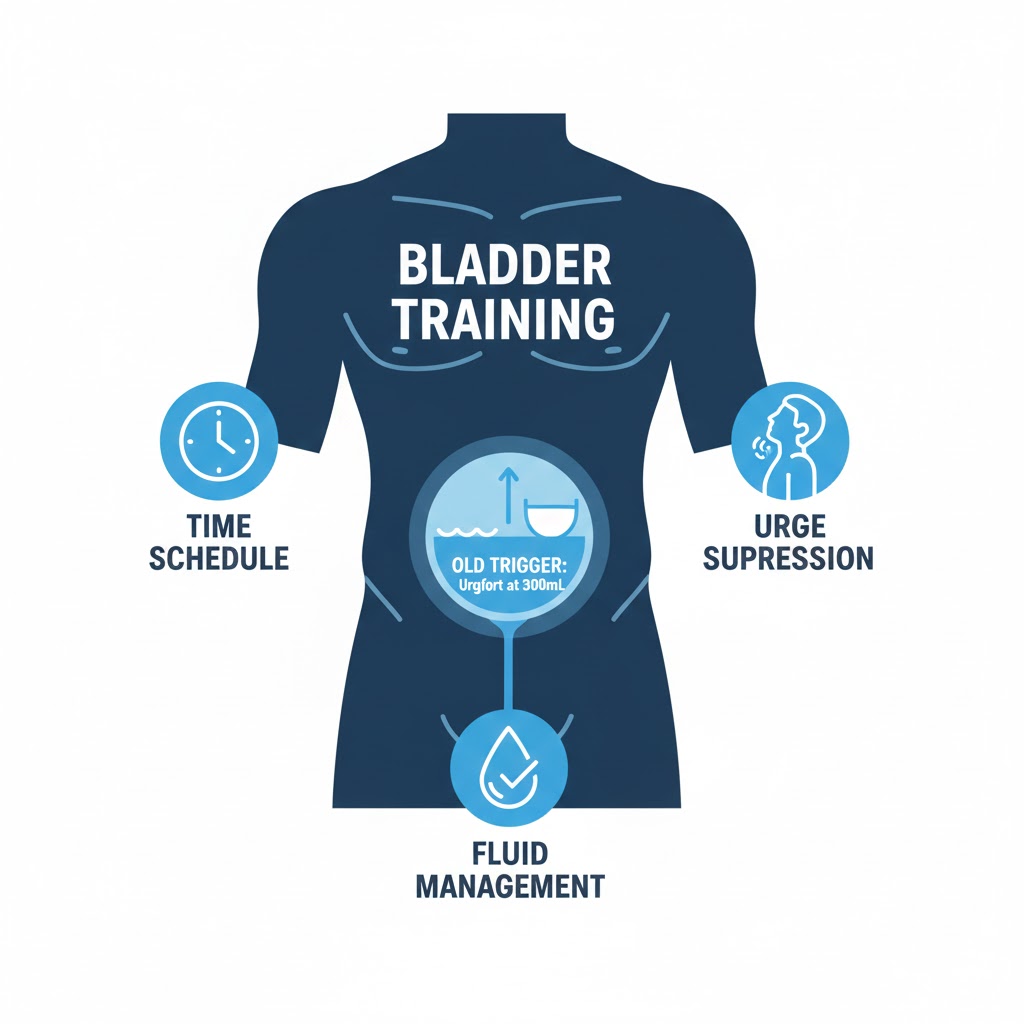
- How it Differs from BPH: Symptoms include straining to urinate, feeling of incomplete emptying, and often urinary frequency because the bladder is never fully emptied. There is little to no urgency (the opposite of an overactive bladder). A key test is measuring post-void residual (PVR) urine via ultrasound—it’s often very high (>300mL).
- Treatment: Intermittent self-catheterization (to empty the bladder), medications to improve contractions (though limited options), treatment of underlying cause.
3. Neurogenic Bladder: The Faulty Wiring
- What it is: Nerve damage disrupts communication between the brain and bladder.
- Common Causes: Spinal cord injury, multiple sclerosis, disc herniation, radical pelvic surgery (for rectal/prostate cancer), long-standing diabetes.
- How it Differs from BPH: Often accompanied by other neurological symptoms (numbness, tingling, leg weakness, bowel changes). Urinary symptoms may include complete inability to urinate (retention), loss of sensation of bladder fullness, and/or urinary incontinence.
- Diagnosis: Neurological exam, urodynamic testing, MRI of spine/brain.
- Treatment: Managed based on the specific nerve pattern—may involve catheterization, medications, or neuromodulation.
4. Medication Side Effects: The Chemical Culprits
- What it is: Numerous medications can impair bladder contraction or increase outlet resistance.
- Common Culprits:
- Anticholinergics: For overactive bladder, allergies, depression (e.g., oxybutynin, diphenhydramine, amitriptyline).
- Decongestants: Pseudoephedrine, phenylephrine (tighten bladder neck).
- Opioid Pain Medications: Suppress neural signals.
- Some Antipsychotics & Antidepressants.
- How it Differs: Symptoms typically begin or worsen soon after starting a new medication. Reviewing your medication list with a doctor or pharmacist is crucial.
5. Pelvic Floor Dysfunction (Hypertonic): The Too-Tight Sling
- What it is: The pelvic floor muscles are chronically tight and unable to relax, paradoxically obstructing urine flow.
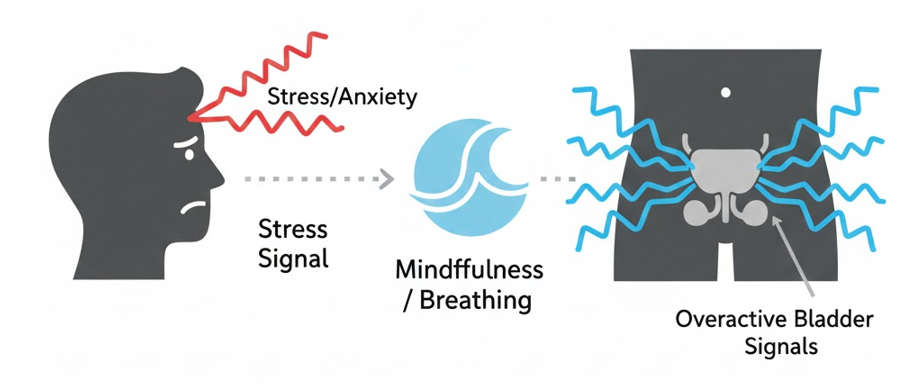
- Common Causes: Chronic straining (from constipation or original BPH), anxiety/stress, protective guarding after pelvic pain or trauma.
- How it Differs from BPH: Often associated with pelvic pain, pain with sitting, and constipation. The stream may start and stop in spurts. There is usually a significant component of urgency and frequency as well, as the tight muscles irritate the bladder. Learn the difference in our guide: Pelvic Floor Exercises for BPH.
- Treatment: Pelvic floor physical therapy (focus on relaxation, not strengthening), biofeedback, stress management.
How Your Urologist Will Tell the Difference: Key Tests
To move from symptom to diagnosis, expect these evaluations:
- Detailed History: Onset, progression, associated symptoms (pain, fever, neurological issues), medication review, past procedures.
- Physical Exam: Including digital rectal exam (DRE) to assess prostate.
- Urinalysis & Culture: Rule out infection.
- Urine Flow Test (Uroflowmetry): Measures speed and pattern of flow. A low, plateau-shaped curve suggests obstruction (BPH/stricture). A low, bell-shaped curve suggests weak bladder muscle.
- Post-Void Residual (PVR) Ultrasound: Measures urine left in bladder after voiding. High PVR suggests underactive bladder or significant obstruction.
- Cystoscopy: A thin camera examines the urethra and bladder. Gold standard for diagnosing strictures and visualizing the prostate.
- Urodynamic Studies: Measures bladder pressure during filling and emptying. Complex but definitive for diagnosing neurogenic or underactive bladder.
What to Do If You Have a Weak Stream: Your Action Plan
- Don’t Self-Diagnose as BPH. Especially if you’re under 50, have a history of UTIs/catheters, or have neurological symptoms.
- Schedule a Urology Consultation. Use our Urologist Appointment Preparation Guide to get ready.
- Bring a Complete Medication List (including over-the-counter and supplements).
- Track Your Symptoms with our BPH Self-Assessment Quiz & Bladder Diary to provide concrete data.
- Ask Specific Questions: “Could this be a urethral stricture or underactive bladder?” “Should we do a cystoscopy or urodynamic test?”
Conclusion: The Importance of Precision in Diagnosis
A weak urine stream is your body’s alarm bell. While BPH is the most common reason it goes off, it’s not the only one. Treating a urethral stricture with BPH medications will fail. Treating an underactive bladder with prostate surgery could be disastrous.
The path to effective treatment begins with an accurate diagnosis. By understanding the full spectrum of possible causes, you become an informed partner in your care, ensuring you and your urologist are solving the right problem from the start.
Remember: In urology, the right treatment depends entirely on the right diagnosis. Don’t settle for assumptions.
Navigate Our Complete BPH Hub:
- Silo 1: BPH Symptoms & Daily Management (You are here)
- Silo 2: Medical & Surgical Treatments
- Silo 3: Natural Remedies & Lifestyle
- Main Hub: The Complete Guide to BPH & Prostate Health
FAQs
1. Can anxiety or stress really cause a weak urine stream?
Yes, indirectly. Chronic stress and anxiety can lead to pelvic floor muscle hypertonicity (excessive tightness). These tense muscles can constrict the urethra, making it difficult to initiate and maintain a strong stream. This is often accompanied by urinary urgency and frequency. It’s a functional, not structural, obstruction.
2. I’m in my 30s with a weak stream. Is it likely BPH?
BPH is very uncommon in your 30s. Other causes are far more probable. Top suspects would be: Urethral stricture (especially if you’ve had a catheter or infection), pelvic floor dysfunction, or the early onset of a neurological issue. A urologist visit is essential to rule these out.
3. What’s the difference between “hesitancy” and a truly weak stream?
Hesitancy refers to difficulty initiating urination—you stand there waiting for the flow to start. A weak stream refers to the poor force and caliber of the flow once it begins. They often occur together (as in BPH), but hesitancy alone might point more toward a neurological or medication issue affecting the “start signal.”
4. Can an underactive bladder be reversed?
It depends on the cause. If it’s due to medication, stopping the drug may reverse it. If it’s from diabetic neuropathy, improving blood sugar control may help stabilize it. If it’s from chronic over-distension (the bladder being stretched too long), timely catheterization can prevent permanent damage. However, age-related or injury-related weakness is often managed, not cured, with intermittent catheterization.
5. How can I tell if my weak stream is from BPH or a stricture?
While definitive diagnosis requires a urologist, clues include:
- Age: Strictures often affect younger men.
- History: Previous catheterization, STIs, or trauma suggests stricture.
- Flow Pattern: A very fine, pencil-like but forceful stream suggests stricture. A dribbling, intermittent stream is more typical of BPH.
- Cystoscopy is the definitive test that visualizes the stricture.
6. Do all these conditions require surgery?
No. Treatment varies dramatically:
- Strictures: May require dilation or surgery.
- Underactive Bladder: Primarily managed with clean intermittent self-catheterization, not surgery.
- Neurogenic Bladder: Managed with catheterization, medications, or devices.
- Medication-Induced: Treated by adjusting or stopping the offending drug.
- Pelvic Floor Dysfunction: Treated with physical therapy, not surgery.
7. Can lifting heavy weights cause a weak urine stream?
It’s not a direct cause, but heavy lifting that involves chronic straining and increased abdominal pressure can contribute to pelvic floor dysfunction over time. It can also potentially exacerbate a urethral stricture if one is already present. Proper breathing technique (exhaling during exertion) is important.
8. Will drinking more water improve a weak stream?
Not if there’s a physical obstruction. Increasing fluid intake will increase urine volume, which may temporarily create a slightly stronger stream due to higher bladder pressure, but it does not address the underlying blockage. It can actually worsen frequency and nocturia. The key is treating the cause, not the symptom.
9. Is a weak stream ever a sign of prostate cancer?
Prostate cancer rarely causes urinary obstruction unless it is very advanced and located in a specific area. Urinary symptoms are much more commonly from BPH. However, a weak stream should prompt a visit to a urologist who will perform appropriate screening (PSA, exam) to rule out cancer as part of the evaluation.
10. What’s the single most important test to figure out the cause?
There isn’t one. It’s a stepwise process. The urine flow test + post-void residual ultrasound is a great non-invasive starting point. If obstruction is suggested and you’re young or have relevant history, cystoscopy is key for strictures. For suspected weak bladder or nerve issues, urodynamic studies are definitive. Your urologist will choose the sequence based on your story.
Related Articles
- Prostatitis vs. BPH: Key Differences in Symptoms: Another condition that can mimic BPH symptoms but requires completely different treatment.
- BPH Self-Assessment Quiz & Symptom Tracker: Quantify your symptoms to bring hard data to your urologist appointment.
- Pelvic Floor Exercises for BPH (Step-by-Step Guide): Learn how to address pelvic floor dysfunction, a common non-BPH cause.
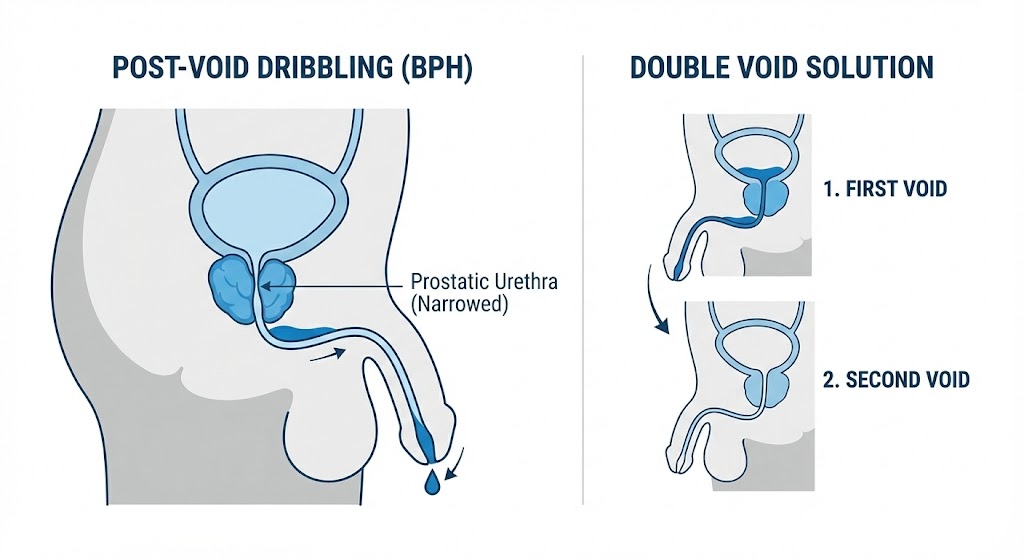
- Post-Void Dribbling: Why It Happens & Solutions: A weak stream often leads to dribbling—here’s how to manage it.
Your Journey to Better Prostate Health Starts Here
This article is just one part of our complete, 30+ article resource on BPH and prostate health.
From first symptoms to treatment recovery, natural remedies to surgical deep dives—we’ve covered it all in one place.
🗺️ Explore The Complete BPH & Prostate Health HubInside: Symptom Trackers | Treatment Comparisons | Recovery Diaries | Diet Plans | FAQs | and much more.
Considering a Natural Prostate Supplement?
Many of our readers have asked about comprehensive natural formulas. Prostavive combines 9 research-backed ingredients including Saw Palmetto, Beta-Sitosterol, and Pygeum in one supplement.
Note: This is an affiliate link. We earn a commission if you purchase, at NO EXTRA COST TO YOU. Always consult your healthcare provider before starting supplements.