IMPORTANT DISCLAIMER: This article is for informational purposes only and is not medical advice. Asthma attacks can be life-threatening. Always use your prescribed rescue inhaler as directed by your doctor. These natural approaches are complementary strategies only and should NEVER replace emergency medical care or prescribed asthma medications.
Feeling that familiar tightening in your chest, the wheeze with each exhale, the rising panic as you struggle to draw a full breath—an asthma attack is a terrifying experience. While your rescue inhaler is your first and most critical line of defense, are there natural approaches that can provide additional relief or help you manage milder symptoms?
This guide explores evidence-based natural strategies that may complement your conventional asthma management. However, let’s be unequivocally clear from the start: Natural remedies are NOT replacements for prescribed asthma medications during an attack. They’re supportive tools that, when used wisely alongside conventional care, may help you breathe more comfortably.
The Golden Rule: Know When It’s an Emergency
STOP READING AND CALL 911 IF:
- Your lips or fingernails are turning blue
- You cannot speak in full sentences
- Your rescue inhaler isn’t helping within 15-20 minutes
- You’re straining your chest muscles to breathe
- You feel confused, drowsy, or exhausted
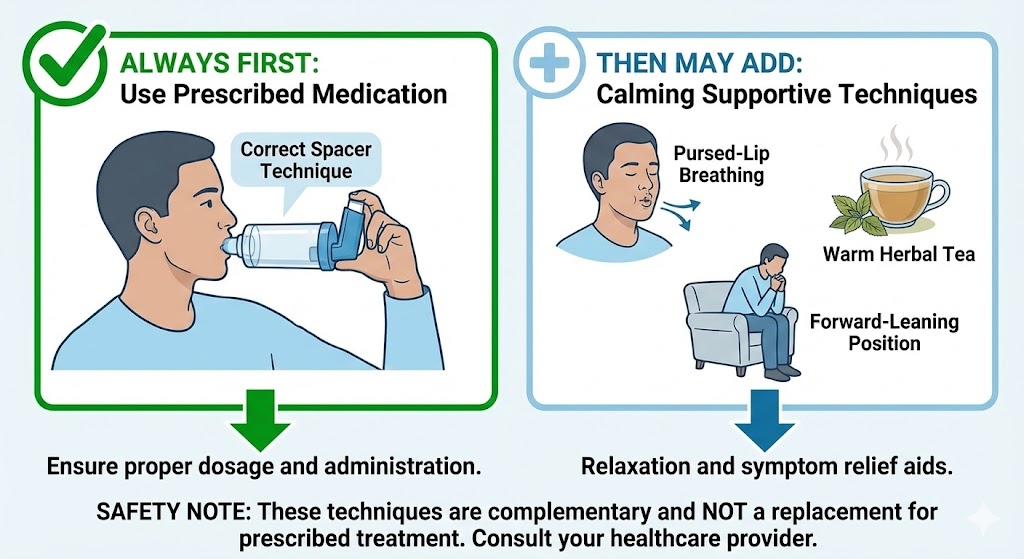
Use Your Rescue Inhaler FIRST, Then Consider These Supports:
- Immediate: Use prescribed rescue medication
- While waiting for medication to work: Try calming techniques
- For milder symptoms between attacks: Consider preventive strategies
- Always: Follow your asthma action plan from your doctor
Immediate Calming Techniques (While Medication Works)
1. The Pursed-Lip Breathing Method
What it does: Slows breathing, keeps airways open longer, reduces panic
How to do it:
- Sit upright, relax your shoulders
- Inhale slowly through your nose for 2 counts
- Purse your lips like you’re whistling
- Exhale slowly through pursed lips for 4-6 counts
- Repeat until breathing eases
Why it helps: Creates back-pressure in airways, preventing them from collapsing during exhalation. This is similar to the technique we discuss in our breathing exercises guide, adapted for acute situations.
2. Forward-Leaning Position
What it does: Uses gravity to help breathing muscles work more efficiently
Options:
- Sitting: Lean forward with elbows on knees
- Standing: Lean forward against a wall or counter
- With support: Place pillow on table, rest head and arms
Why it helps: Reduces work of accessory breathing muscles, allowing diaphragm to work more effectively.
3. Progressive Muscle Relaxation (During Recovery)
What it does: Reduces anxiety that exacerbates asthma symptoms
How to do it:
- After using medication, sit comfortably
- Tense then relax each muscle group (feet → face)
- Focus on releasing chest and shoulder tension
- Combine with slow, deep breathing
Why it helps: Anxiety and asthma create a vicious cycle. Breaking the tension can help medication work more effectively.
Natural Supplements with Potential Bronchodilator Effects
CRITICAL NOTE: These are for prevention and mild symptom support only, NOT acute attacks. Always discuss with your doctor before adding supplements.
1. Magnesium
Evidence: Intravenous magnesium is used in emergency rooms for severe asthma attacks. Oral magnesium may help prevent attacks.
For prevention:
- Dose: 200-400mg magnesium glycinate/citrate daily
- Timing: With meals to avoid digestive upset
- Mechanism: Helps relax bronchial smooth muscles
Caution: Can interact with some medications; start low.
2. Omega-3 Fatty Acids
Evidence: Anti-inflammatory effects may reduce airway inflammation over time
Sources:
- Fish oil: 1000-2000mg EPA+DHA daily
- ALA sources: Flaxseed, chia seeds, walnuts
- Consistency: Daily use for cumulative effect
Why it helps: May reduce frequency and severity of attacks when used consistently as part of a comprehensive approach like those in our asthma supplements guide.
3. Vitamin D
Evidence: Low vitamin D linked to increased asthma severity
For prevention:
- Testing: Get levels checked first
- Dose: Typically 1000-4000 IU daily (based on levels)
- Form: D3 with K2 for better absorption
Why it helps: Modulates immune response, may reduce steroid needs in some patients.
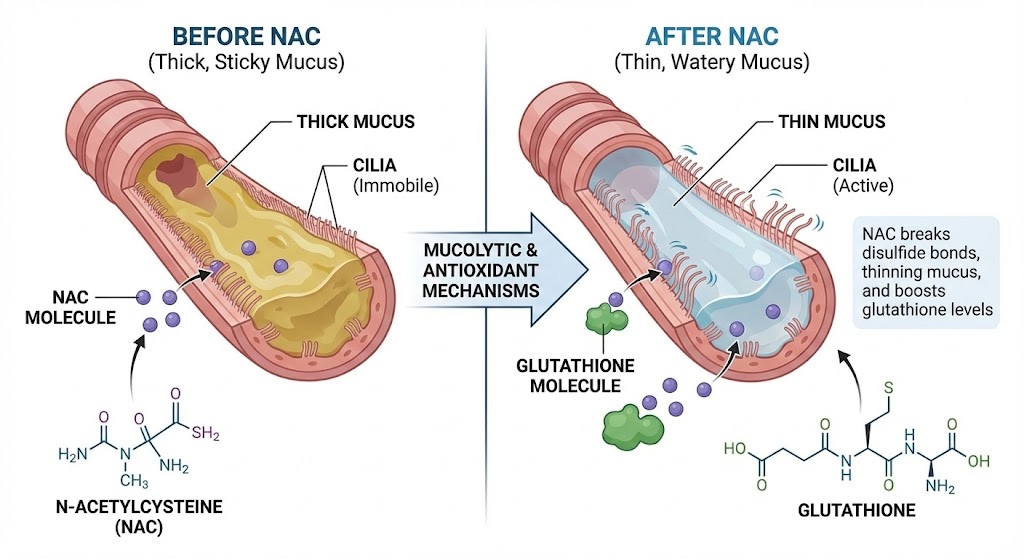
4. NAC (N-Acetyl Cysteine)
Evidence: Thins mucus, antioxidant effects (read our full NAC guide for details)
Important distinction: For mucus clearance between attacks, NOT for acute bronchospasm relief.
Herbal Approaches with Cautions
1. Ginger
Potential benefits: Natural anti-inflammatory, may help relax airways
Forms:
- Fresh ginger tea: 1-inch piece sliced, steeped 10 minutes
- Powder: 1-2 grams daily in divided doses
- Standardized extract: Follow product instructions
Caution: May interact with blood thinners; can cause heartburn.
2. Turmeric (Curcumin)
Evidence: Potent anti-inflammatory, may reduce airway inflammation
For effectiveness:
- Must include: Black pepper (piperine) or lipids for absorption
- Dose: 500-1000mg curcumin with piperine daily
- Timing: With fatty meals
Why it helps: Reduces inflammatory mediators that contribute to asthma pathophysiology.
3. Thyme
Traditional use: For cough and bronchial spasm
Safe forms during mild symptoms:
- Tea: 1-2 cups daily of weak thyme tea
- Steam inhalation: For chest tightness (not during acute attack)
- Honey combination: Thyme-infused honey for cough
Critical: NOT for acute attacks; some asthmatics are sensitive to strong herbs.
4. Butterbur (Petasites hybridus)
Evidence: Some studies show reduction in asthma symptoms
MAJOR CAUTION:
- Must be: PA-free (pyrrolizidine alkaloids removed)
- Only use: Certified PA-free products
- Avoid: Raw butterbur or uncertified supplements
Why limited use: Safety concerns outweigh benefits for most asthmatics.
Environmental Triggers: Immediate Response
1. Steam/Humidity
For: Cough-variant asthma or mucus-related symptoms
Method:
- Hot shower with door closed
- Humidifier with distilled water
- Bowl of hot water with towel tent (add drop of eucalyptus if tolerated)
Why it helps: Moist air can soothe irritated airways and loosen mucus.
2. Cold Air Protection
For: Exercise-induced or cold-air triggered asthma
Immediate response:
- Breathe through scarf or mask
- Cover nose and mouth
- Move to warmer environment
Why it helps: Warming and humidifying air before it hits sensitive airways.
3. Allergen Removal
For: Allergy-induced asthma attacks
Quick actions:
- Pets: Remove from room immediately
- Dust: Leave room, use air purifier
- Pollen: Close windows, shower immediately
- Mold: Leave damp areas
Why it helps: Removing trigger reduces ongoing immune response.
Dietary Considerations During Recovery
Foods That May Help (Long-term):
- Anti-inflammatory foods: Fatty fish, berries, leafy greens
- Magnesium-rich: Spinach, pumpkin seeds, almonds
- Vitamin C sources: Citrus, bell peppers, broccoli
- Quercetin sources: Onions, apples, capers (natural mast cell stabilizer)
Foods to Avoid During Flare-ups:
- Sulfites: Dried fruits, wine, processed potatoes
- Histamine-rich: Aged cheeses, fermented foods, alcohol
- Common allergens: Dairy, eggs, nuts (if you’re sensitive)
- Cold beverages: Can trigger bronchospasm in some
Hydration Importance:
- Water: Essential for thinning mucus
- Warm liquids: Herbal teas can be soothing
- Avoid: Sugary drinks that may increase inflammation
What NOT to Do During an Asthma Attack
Dangerous Misconceptions:
- ❌ Drinking coffee as emergency treatment (minimal effect, delays real treatment)
- ❌ Essential oils in nebulizer (can cause severe bronchospasm)
- ❌ Over-the-counter cough medicines (may suppress needed cough reflex)
- ❌ Holding breath or hyperventilating (worsens symptoms)
- ❌ Lying flat (makes breathing more difficult)
Supplement Red Flags During Attacks:
- ❌ Ephedra/Ma Huang (dangerous stimulant, banned in US)
- ❌ High-dose vitamin C (can cause diarrhea, dehydration)
- ❌ Unregulated herbal combinations (unknown interactions)
- ❌ Anything marketed as “natural inhaler” (not proven, delays care)
Creating Your Natural Support Plan (Between Attacks)
Step 1: Work With Your Doctor
- Discuss which natural approaches are safe for you
- Get allergy testing if needed
- Create a written asthma action plan
- Regular lung function monitoring
Step 2: Build Your Prevention Toolkit
Daily:
- Appropriate supplements (based on testing/discussion)
- Anti-inflammatory diet
- Stress management techniques
Seasonal:
- Allergy management plan
- Immune support during cold/flu season
- Environmental adjustments
Step 3: Know Your Triggers
Common triggers to identify:
- Allergens (pollen, dust mites, pet dander)
- Irritants (smoke, pollution, strong odors)
- Weather changes (cold air, humidity, storms)
- Exercise (manage with proper warm-up)
- Stress and strong emotions
- Respiratory infections
Step 4: Track and Adjust
Keep a journal:
- Symptoms, severity, duration
- Potential triggers
- What helped/worsened symptoms
- Medication use
- Supplement effects
When Natural Approaches Make Sense
Appropriate Use:
- Prevention: Reducing frequency of attacks
- Mild symptoms: Between attacks, with doctor approval
- Recovery support: After attack, alongside medical care
- Trigger management: Environmental controls
- Stress reduction: Complementary to medical treatment
Inappropriate Use:
- During moderate-severe attacks: Delay medical care
- Instead of prescribed medications: Dangerous substitution
- Without doctor knowledge: Risk of interactions
- For life-threatening symptoms: Requires emergency care
Special Considerations
For Children:
- Extra caution: More vulnerable to severe attacks
- Pediatrician consultation: Essential before any natural approach
- Honey caution: Not under 1 year old
- Dose adjustments: Based on weight/age
For Elderly:
- Multiple medications: Higher interaction risk
- Comorbid conditions: May complicate asthma management
- Weaker immune response: Caution with immune-modulating herbs
- Monitoring: More frequent check-ups needed
Pregnancy/Breastfeeding:
- Limited safety data: For most natural approaches
- Essential: Doctor guidance for any supplement/herb
- Priority: Well-controlled asthma for baby’s health
- Avoid: Ephedra, high-dose vitamins, questionable herbs
The Reality Check: What Actually Works Evidence-Based
Strong Evidence For:
- Breathing techniques (as adjunct, not replacement)
- Trigger avoidance (environmental controls)
- Magnesium IV (in hospital for severe attacks)
- Vitamin D (for deficiency correction)
- Omega-3s (modest reduction in inflammation)
Weak or Mixed Evidence For:
- Most herbal remedies (individual responses vary)
- Acupuncture (may help some, not emergency treatment)
- Homeopathy (no scientific evidence for acute attacks)
- Most “alternative” inhalers (not FDA-approved, risky)
Proven Harmful:
- Delaying conventional treatment
- Unproven “cures” instead of medications
- Essential oils in airways (chemical pneumonitis risk)
- Stimulant herbs during attacks (increases stress on heart)
Building a Safe, Integrated Approach
Your Asthma Management Should Include:
- Foundation: Prescribed medications (controller and rescue)
- Prevention: Trigger identification and avoidance
- Support: Evidence-based natural approaches (with doctor approval)
- Monitoring: Regular check-ups and lung function tests
- Emergency plan: Clear steps for worsening symptoms
Sample Integrated Daily Plan:
Morning:
- Controller medication (if prescribed)
- Vitamin D (if deficient, with doctor approval)
- Anti-inflammatory breakfast
Throughout day:
- Stay hydrated
- Avoid known triggers
- Stress management breaks
Evening:
- Omega-3 supplement (with doctor approval)
- Relaxation techniques
- Clean sleeping environment
As needed:
- Rescue inhaler for symptoms
- Steam for chest tightness
- Pursed-lip breathing for mild breathlessness
Final Words: Empowerment Through Knowledge, Not Replacement
Asthma is a serious medical condition that requires conventional medical treatment. Natural approaches can play a supportive role when used:
- Wisely (with proper knowledge)
- Safely (under medical supervision)
- Appropriately (as complement, not replacement)
- Evidence-based (relying on science, not anecdotes)
Your best defense against asthma attacks remains:
- A good relationship with your healthcare provider
- Proper use of prescribed medications
- A personalized asthma action plan
- Knowing when to seek emergency care
Natural remedies have their place in a comprehensive asthma management strategy, but that place is alongside conventional care, not instead of it. For more resources on managing respiratory conditions naturally and safely, explore our lung health resource hub.
Remember: When in doubt during an asthma attack, use your rescue medication and seek medical attention. It’s always better to be safe with asthma.
FAQs
1. Can I use essential oils during an asthma attack?
Absolutely not. Essential oils can trigger severe bronchospasm and chemical pneumonitis when inhaled directly, especially during an asthma attack. Some asthmatics may tolerate diffused oils when well-controlled, but never during symptoms. Never put oils in nebulizers or steam inhalers during attacks.
2. Is coffee an emergency treatment for asthma attacks?
No. While caffeine has mild bronchodilator effects, it’s not nearly strong enough for an asthma attack. Relying on coffee delays proper treatment with rescue medications. The American Lung Association does NOT recommend coffee as asthma emergency treatment.
3. Can breathing exercises stop an asthma attack?
Breathing techniques like pursed-lip breathing can help manage mild symptoms and reduce panic, but they cannot stop a moderate to severe asthma attack. Always use your rescue inhaler first for any asthma symptoms, then use breathing techniques while waiting for medication to work.
4. Are there any natural alternatives to steroid inhalers?
No proven natural alternatives exist that match the effectiveness of inhaled corticosteroids for controlling airway inflammation. Some natural approaches may help reduce inflammation modestly, but they should not replace prescribed controller medications. Always discuss any changes with your doctor.
5. How can I naturally prevent nighttime asthma attacks?
Evidence-based approaches include: using mattress/pillow covers for dust mites, keeping pets out of bedroom, using air purifier, elevating head of bed, managing GERD (common asthma trigger), and taking prescribed medications as directed. Natural supplements should only be added with doctor approval.
6. Can diet cure my asthma?
No diet can cure asthma. However, an anti-inflammatory diet may help reduce overall inflammation and potentially decrease asthma severity for some people. Elimination diets may help if you have specific food allergies triggering asthma, but this requires medical supervision.
7. Are herbal teas safe during asthma attacks?
Warm herbal teas may provide psychological comfort but offer no significant bronchodilation during an attack. Some teas (chamomile, echinacea) can actually trigger allergic reactions in sensitive individuals. During an attack, focus on your rescue medication, not tea.
8. Can meditation prevent asthma attacks?
While meditation won’t prevent attacks caused by allergens or infections, it can help manage stress-induced asthma. Since stress can trigger attacks in some people, stress reduction techniques may reduce frequency of stress-related flare-ups as part of a comprehensive management plan.
9. Is it safe to exercise during mild asthma symptoms?
No. Exercise with any asthma symptoms can worsen bronchospasm. Use your rescue inhaler before exercise if prescribed, and only exercise when completely symptom-free. If symptoms develop during exercise, stop immediately and use rescue medication.
10. How do I know if a natural remedy is interacting with my asthma medications?
Always: 1) Research potential interactions before trying anything new, 2) Discuss all supplements with your doctor and pharmacist, 3) Start with low doses to check tolerance, 4) Monitor for unusual symptoms. Common interactions include blood thinners with anti-inflammatory herbs and steroids with immune-stimulating supplements.
“`