That unsettling feeling of not being able to catch your breath—whether it comes on suddenly during exertion or lingers as a constant background discomfort—can be both physically limiting and emotionally distressing. Shortness of breath (medically known as dyspnea) isn’t a condition itself but a symptom with many possible causes, from asthma and COPD to anxiety, anemia, or even deconditioning.
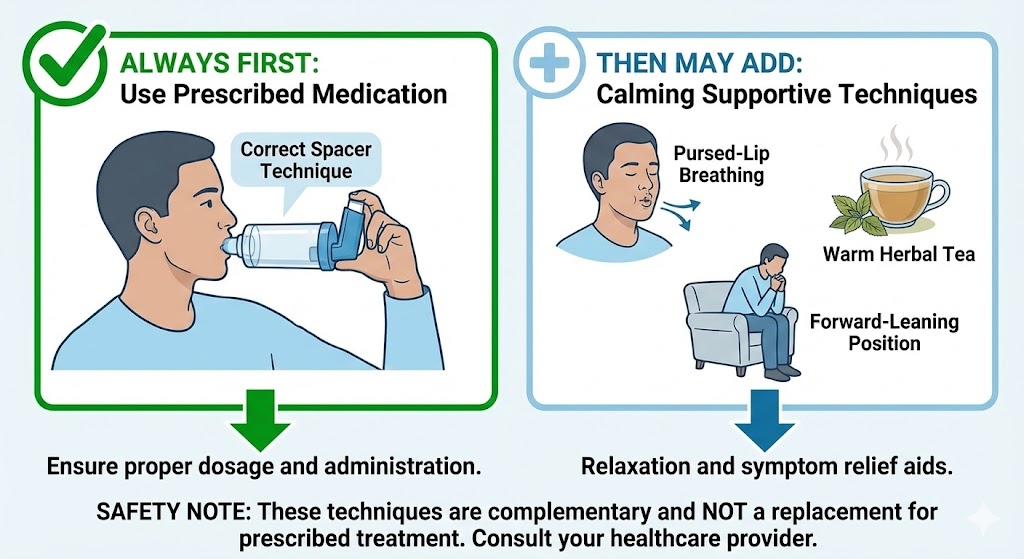
While it’s crucial to identify and address the underlying cause with medical guidance, there are natural approaches that can help you breathe more comfortably. These strategies don’t replace medical treatment but can complement it, helping you manage symptoms and improve your quality of life.
This guide explores evidence-based natural strategies and supplements that may help you manage shortness of breath, whether it stems from respiratory conditions, cardiovascular issues, or other factors. For a comprehensive understanding of different types of breathlessness, see our guide on the 3 types of shortness of breath.
First Steps: Understanding Your Shortness of Breath
Red Flags: When to Seek Immediate Medical Attention
STOP and call 911 or go to the emergency room if you experience:
- Sudden, severe shortness of breath
- Chest pain, pressure, or tightness
- Fainting or near-fainting
- Blue lips or fingernails
- Confusion or inability to speak in full sentences
- Rapid heart rate with breathing difficulty
Common Causes of Chronic Shortness of Breath:
- Respiratory conditions: Asthma, COPD, pulmonary fibrosis
- Cardiovascular issues: Heart failure, arrhythmias
- Anemia: Low red blood cell count
- Anxiety/Panic disorders: Hyperventilation syndrome
- Deconditioning: Poor physical fitness
- Obesity: Excess weight putting pressure on lungs
- GERD/Silent reflux: As discussed in our silent reflux article
Important: Always get a proper diagnosis before trying natural approaches. What helps cardiac-related breathlessness may differ from respiratory causes.
Breathing Techniques for Immediate Relief
1. Pursed-Lip Breathing (Gold Standard for COPD/Asthma)
What it does: Slows breathing rate, keeps airways open longer, reduces air trapping
How to practice:
- Sit comfortably with shoulders relaxed
- Inhale slowly through your nose for 2 counts
- Purse lips as if whistling or blowing out a candle
- Exhale slowly through pursed lips for 4-6 counts
- Repeat for 5-10 minutes, several times daily
Evidence: Shown to improve oxygen saturation, reduce respiratory rate, and decrease anxiety in COPD patients.
2. Diaphragmatic Breathing (Belly Breathing)
What it does: Strengthens diaphragm, improves breathing efficiency
Training method:
- Lie on back with knees bent or sit comfortably
- Place one hand on chest, one on abdomen
- Inhale through nose, feeling abdomen rise (chest should move minimally)
- Exhale through pursed lips, feeling abdomen fall
- Practice 5-10 minutes daily
Benefit: Reduces work of breathing, especially helpful for anxiety-related breathlessness.
3. Box Breathing (For Anxiety-Induced Shortness)
What it does: Regulates nervous system, reduces panic
Pattern:
- Inhale for 4 counts
- Hold for 4 counts
- Exhale for 4 counts
- Hold for 4 counts
- Repeat for several cycles
When to use: At first signs of anxiety-related breathlessness, or as daily practice to reduce baseline anxiety.
4. Positioning Techniques
Tripod position: Lean forward with arms on knees or table
High side-lying: Lie on side with head elevated on pillows
Supported forward lean: Against wall with feet slightly away
Mechanism: Uses gravity to help breathing muscles work more efficiently.
Evidence-Based Supplements for Respiratory Support
1. Magnesium
How it helps: Natural bronchodilator, relaxes smooth muscles in airways
For respiratory shortness:
- Form: Magnesium glycinate or citrate (better absorbed)
- Dose: 200-400mg daily (with meals)
- Timing: Split doses if causing loose stools
- Evidence: Intravenous magnesium used in ER for asthma attacks; oral may help prevent
Caution: May interact with some medications; start low.
2. Omega-3 Fatty Acids
How they help: Reduce inflammation in airways and blood vessels
For inflammatory conditions:
- Source: Fish oil (EPA+DHA) or algal oil
- Dose: 1000-2000mg combined EPA+DHA daily
- Quality: Look for third-party tested, purified
- Timeframe: Effects build over 4-12 weeks
Research: May improve exercise tolerance in COPD and reduce asthma symptoms.
3. Coenzyme Q10 (CoQ10)
How it helps: Improves cellular energy production, antioxidant
Particularly helpful for:
- Cardiac-related breathlessness
- Those on statin medications (deplete CoQ10)
- Age-related decline in mitochondrial function
Dosing:
- Ubiquinol form: 100-200mg daily (better absorbed)
- With fats: Take with meals containing fat
- Timing: Consistency more important than specific time
4. Iron (Only if Deficient)
Critical: Only supplement if blood tests confirm deficiency
How it helps: Essential for oxygen transport in hemoglobin
If deficient:
- Form: Iron bisglycinate (gentler on stomach)
- With: Vitamin C to enhance absorption
- Avoid with: Calcium, coffee, tea (inhibit absorption)
- Monitor: Follow-up blood tests in 2-3 months
Warning: Never supplement iron without testing—excess iron is dangerous.
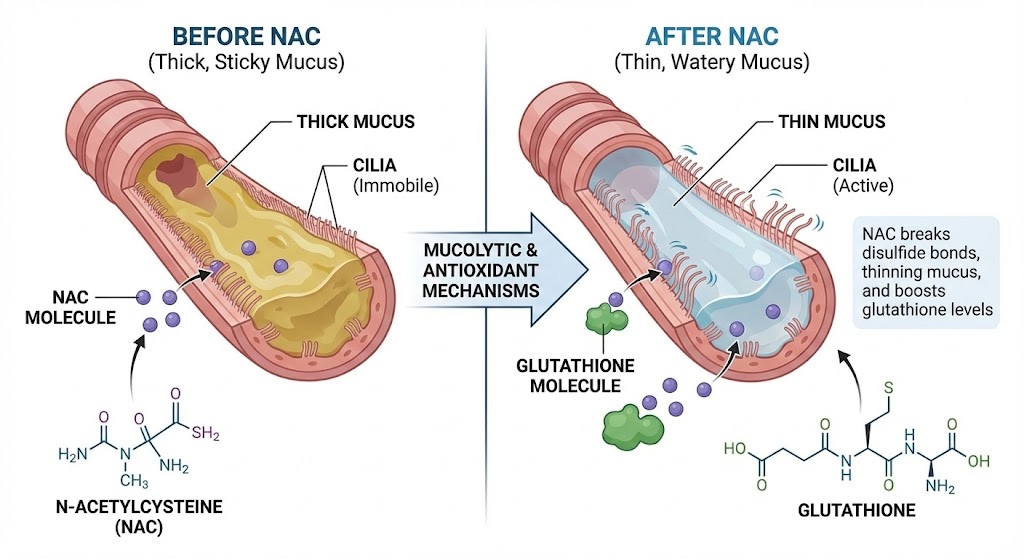
5. NAC (N-Acetyl Cysteine)
How it helps: Thins mucus, boosts glutathione (master antioxidant)
For mucus-related breathlessness:
- Dose: 600-1200mg daily (split doses)
- Timing: With food to reduce stomach upset
- Evidence: Reduces COPD exacerbations by 25-30%
Note: More for chronic mucus clearance than acute breathlessness.
6. L-Carnitine
How it helps: Improves muscle energy metabolism, including respiratory muscles
For exercise-induced breathlessness:
- Form: L-carnitine L-tartrate or acetyl-L-carnitine
- Dose: 1000-2000mg daily
- Timing: Before exercise for performance benefit
- Research: May improve exercise tolerance in COPD and heart failure
Herbal Approaches with Scientific Support
1. Thyme
Benefits: Expectorant, antimicrobial, anti-inflammatory
For respiratory infections causing breathlessness:
- Form: Tea (1-2 tsp dried herb per cup)
- Steam inhalation: For chest congestion
- Timing: At first signs of infection
- Caution: Not for acute asthma attacks
2. Ginger
Benefits: Anti-inflammatory, may help relax airways
Forms:
- Fresh tea: 1-inch piece sliced, steeped 10 minutes
- Powder: 1-2 grams daily in divided doses
- Standardized extract: Follow product instructions
Research: May improve asthma control and reduce airway inflammation.
3. Turmeric (Curcumin)
Benefits: Potent anti-inflammatory comparable to some medications
For effectiveness:
- Must include: Black pepper (piperine) or fats for absorption
- Dose: 500-1000mg curcumin with piperine daily
- Quality: Look for high-curcuminoid extracts
- Time: Consistent daily use for cumulative effect
4. Ginseng (Asian Ginseng)
Benefits: May improve exercise tolerance, reduce fatigue
For breathlessness with fatigue:
- Form: Standardized extract (4-7% ginsenosides)
- Dose: 200-400mg daily
- Cycling: 2-3 weeks on, 1-2 weeks off
- Caution: Can interact with medications, affect blood pressure
Dietary Strategies for Better Breathing
Anti-Inflammatory Eating Pattern
Focus on:
- Fatty fish: Salmon, mackerel, sardines (2-3 times weekly)
- Colorful fruits/vegetables: Berries, leafy greens, cruciferous veggies
- Healthy fats: Olive oil, avocados, nuts, seeds
- Whole grains: Oats, quinoa, brown rice
- Lean proteins: Chicken, turkey, legumes
Limit:
- Processed foods high in sodium (can cause fluid retention)
- Inflammatory oils (soybean, corn, vegetable oils)
- Sugar and refined carbohydrates
- Dairy (if it increases mucus production for you)
Hydration for Thinner Mucus
Goal: Adequate hydration keeps respiratory secretions thin
Guidelines:
- Water: At least 8 cups daily, more if active or in dry climate
- Herbal teas: Peppermint, ginger, thyme
- Broth-based soups: Especially helpful during illness
- Monitor urine: Pale yellow indicates good hydration
Caution: Heart failure patients may need fluid restriction—follow doctor’s advice.
Small, Frequent Meals
Why it helps: Large meals can push up on diaphragm, limiting lung expansion
Strategy:
- 5-6 smaller meals instead of 3 large ones
- Eat slowly, chew thoroughly
- Avoid lying down for 2-3 hours after eating
- Especially important with GERD/silent reflux
Lifestyle Modifications for Long-Term Improvement
1. Gradual Exercise Training
Paradox: Exercise can cause breathlessness but also improves it long-term
Safe approach:
- Start slow: 5-10 minutes daily, increase gradually
- Interval training: Alternate activity with rest periods
- Pursed-lip breathing: During exertion
- Listen to body: Stop if severely breathless or dizzy
Best exercises: Walking, stationary cycling, swimming, tai chi
2. Weight Management
Mechanism: Excess weight:
- Increases oxygen demand
- Puts mechanical pressure on lungs
- Often coexists with sleep apnea
Strategy: Even 5-10% weight loss can significantly improve breathlessness
3. Sleep Optimization
Connection: Poor sleep worsens daytime breathlessness
For better sleep breathing:
- Elevate head of bed
- Address sleep apnea if present
- Maintain consistent sleep schedule
- Create allergen-free sleep environment
4. Stress Reduction Techniques
Mind-body connection: Anxiety directly affects breathing patterns
Daily practices:
- Meditation (even 10 minutes daily)
- Gentle yoga or stretching
- Progressive muscle relaxation
- Nature exposure (“forest bathing”)
Environmental Controls
1. Air Quality Management
Indoor:
- HEPA air purifier
- Regular vacuuming with HEPA filter
- Humidity control (40-50% ideal)
- Natural cleaning products
Outdoor:
- Check air quality index daily
- Limit outdoor activity on poor air days
- Wear mask if necessary in polluted areas
2. Allergen Reduction
Common triggers: Dust mites, mold, pet dander, pollen
Strategies:
- Allergy-proof bedding covers
- Regular mold inspection
- HEPA vacuum and air filters
- Pet restrictions in bedroom
3. Temperature and Humidity Control
Cold, dry air: Can trigger bronchospasm
Hot, humid air: Feels harder to breathe
Solutions:
- Scarf over face in cold weather
- Air conditioning in heat/humidity
- Humidifier in dry environments (clean regularly!)
When to Use Which Strategy
Based on Cause:
For Asthma/COPD:
- Breathing techniques (pursed-lip, diaphragmatic)
- Magnesium supplementation
- Omega-3 anti-inflammatory support
- Environmental trigger control
- Maintain healthy weight
For Cardiac-Related Breathlessness:
- CoQ10 (especially if on statins)
- Omega-3 for inflammation
- Iron if anemic (test first!)
- Sodium/fluid restriction if advised
- Gradual, supervised exercise
For Anxiety-Induced Breathlessness:
- Box breathing and meditation
- Magnesium (calming mineral)
- Regular exercise
- Cognitive behavioral approaches
- Limit caffeine and stimulants
For Deconditioning:
- Graduated exercise program
- Protein for muscle maintenance
- B vitamins for energy metabolism
- Stay hydrated
- Pace activities
Monitoring Your Progress
Track These Metrics:
- Breathlessness scale: Rate daily (0-10 scale)
- Activity tolerance: How far/long can you walk without stopping?
- Medication use: Rescue inhaler or other medication frequency
- Sleep quality: How rested do you feel?
- Energy levels: Throughout the day
Red Flags to Report to Doctor:
- Worsening symptoms despite interventions
- New swelling in legs/ankles
- Chest pain with breathlessness
- Unexplained weight loss
- Fever with breathing difficulties
Safety Considerations and Interactions
Supplement-Drug Interactions:
- Magnesium: Can interact with certain antibiotics, osteoporosis drugs
- Omega-3s: May increase bleeding risk with blood thinners
- CoQ10: May affect warfarin dosing
- Iron: Can interact with thyroid medications, antibiotics
- Always discuss supplements with your healthcare provider
Herbal Cautions:
- Ginseng: Can affect blood pressure, blood sugar, interact with stimulants
- Licorice root: Can raise blood pressure, deplete potassium
- Ephedra/Ma Huang: Dangerous, banned in US—avoid completely
- Quality matters: Choose reputable brands with third-party testing
Building Your Personalized Plan
Step 1: Medical Foundation
- Get proper diagnosis
- Optimize prescribed treatments
- Regular follow-ups with healthcare provider
Step 2: Start with Basics
- Master breathing techniques
- Optimize diet and hydration
- Begin gentle movement
- Improve sleep environment
Step 3: Add Supplements Strategically
- Start with one at a time
- Begin with lowest effective dose
- Monitor for benefits and side effects
- Give each 4-8 weeks before assessing
Step 4: Track and Adjust
- Keep symptom journal
- Regular reassessment with provider
- Adjust based on response
- Be patient—some benefits take months
When Natural Approaches Aren’t Enough
Signs You Need Medical Re-evaluation:
- Symptoms worsening despite interventions
- New or concerning symptoms developing
- Unable to perform activities of daily living
- Frequent nighttime awakening with breathlessness
- Depression or anxiety about breathing worsening
The Role of Pulmonary Rehabilitation:
What it is: Supervised program combining exercise, education, and support
Benefits: Proven to improve quality of life, reduce breathlessness, increase exercise tolerance
Consider if: You have chronic lung condition affecting daily life
Long-Term Mindset: Management, Not Cure
For most chronic causes of breathlessness, the goal is:
- Better management, not elimination
- Improved quality of life
- Increased activity tolerance
- Reduced anxiety about breathing
- Fewer exacerbations
Maintenance Phase:
- Consistency with helpful strategies
- Regular monitoring of symptoms
- Periodic reassessment with healthcare team
- Adjustments as needed with aging/changing health
Final Perspective: Empowerment Through Holistic Care
Shortness of breath can make you feel powerless, but taking a comprehensive, multi-faceted approach can restore a sense of control. Remember:
- Medical care is foundation: Always work with your healthcare team
- Natural supports complement: They’re additions, not replacements
- Individual responses vary: What helps one person may not help another
- Patience is required: Some benefits accumulate slowly
- Quality of life matters: Even small improvements are valuable
By combining evidence-based natural approaches with conventional medical care, you can create a personalized strategy to breathe more comfortably and live more fully. For more resources on comprehensive respiratory health, explore our lung health resource hub.
Remember: The goal isn’t necessarily to eliminate all breathlessness (which may not be possible with certain conditions), but to minimize its impact on your life and maximize your ability to do what matters to you.
FAQs
1. What’s the fastest natural relief for shortness of breath?
Pursed-lip breathing often provides the quickest relief for respiratory-related breathlessness. Sit upright, inhale slowly through your nose for 2 counts, then exhale slowly through pursed lips for 4-6 counts. Repeat for several minutes. This creates back-pressure that keeps airways open longer. However, if breathlessness is severe or accompanied by chest pain, seek immediate medical attention.
2. Can anxiety really cause shortness of breath?
Absolutely. Anxiety triggers the “fight or flight” response, causing rapid, shallow breathing (hyperventilation) that can lead to feelings of breathlessness, chest tightness, and even panic. This creates a vicious cycle where breathlessness causes more anxiety. Techniques like box breathing (inhale-hold-exhale-hold for equal counts) can help break this cycle.
3. Which supplements are best for COPD-related shortness of breath?
Evidence supports: 1) NAC (600-1200mg daily) to reduce mucus and exacerbations, 2) Omega-3s (1000-2000mg EPA+DHA) to reduce inflammation, 3) Vitamin D if deficient (test first), 4) Magnesium (200-400mg daily) as a natural bronchodilator. Always discuss with your doctor before starting supplements.
4. How can I distinguish between heart-related and lung-related breathlessness?
While only a doctor can diagnose definitively, patterns differ: Heart-related often worsens when lying flat (orthopnea) or at night (paroxysmal nocturnal dyspnea), may include leg swelling. Lung-related often includes cough, wheezing, mucus production, and may be triggered by allergens or irritants. Our guide on types of shortness of breath provides more detail.
5. Is it safe to exercise when I get short of breath easily?
Yes, with careful planning. Start with very short sessions (5-10 minutes) of low-intensity activity like walking. Use pursed-lip breathing during exertion. Stop if you become severely breathless, dizzy, or have chest pain. Gradually increase duration and intensity over weeks to months. Pulmonary rehabilitation programs provide supervised, safe exercise for those with significant limitations.
6. Can diet really affect my breathing?
Significantly. An anti-inflammatory diet (rich in fruits, vegetables, fatty fish, whole grains) can reduce systemic inflammation that affects airways. Small, frequent meals prevent abdominal pressure on the diaphragm. Adequate hydration keeps mucus thin. Limiting sodium helps prevent fluid retention that can worsen cardiac-related breathlessness.
7. How long do natural approaches take to work?
It varies: Breathing techniques can provide immediate relief during episodes. Dietary changes may show effects in days to weeks. Most supplements need 4-12 weeks of consistent use to demonstrate benefits. Exercise tolerance improves over months of consistent training. Be patient and consistent.
8. Are there any natural approaches I should avoid?
Yes: 1) Essential oils in airways (can trigger bronchospasm), 2) Ephedra/Ma Huang (dangerous, banned), 3) High-dose caffeine as emergency treatment (delays real care), 4) Breath-holding exercises if you have certain heart/lung conditions, 5) Cold water immersion if you have cardiac issues. When in doubt, consult your doctor.
9. Can posture affect my breathing?
Absolutely. Slumped posture compresses lungs and diaphragm. Sitting or standing upright expands lung capacity. The “tripod position” (leaning forward with arms on knees) helps breathing muscles work more efficiently. Sleeping with head elevated can prevent nighttime breathlessness. Consider posture correction exercises if you have forward head/rounded shoulders.
10. When should I stop natural approaches and see a doctor?
Immediately if: symptoms suddenly worsen, you develop chest pain, fever, coughing up blood, blue lips/nails, confusion, or can’t speak in full sentences. Schedule an appointment if: symptoms gradually worsen despite interventions, you need more rescue medication, sleep is frequently disrupted, or anxiety about breathing is increasing.